Makindo Medical Notes.com |
|
|---|---|
| Download all this content in the Apps now Android App and Apple iPhone/Pad App | |
| MEDICAL DISCLAIMER:The contents are under continuing development and improvements and despite all efforts may contain errors of omission or fact. This is not to be used for the assessment, diagnosis or management of patients. It should not be regarded as medical advice by healthcare workers or laypeople. It is for educational purposes only. Please adhere to your local protocols. Use the BNF for drug information. If you are unwell please seek urgent healthcare advice. If you do not accept this then please do not use the website. Makindo Ltd | |
Guillain Barre Syndrome
-
| About | Anaesthetics and Critical Care | Anatomy | Biochemistry | Cardiology | Clinical Cases | CompSci | Crib | Dermatology | Differentials | Drugs | ENT | Electrocardiogram | Embryology | Emergency Medicine | Endocrinology | Ethics | Foundation Doctors | Gastroenterology | General Information | General Practice | Genetics | Geriatric Medicine | Guidelines | Haematology | Hepatology | Immunology | Infectious Diseases | Infographic | Investigations | Lists | Microbiology | Miscellaneous | Nephrology | Neuroanatomy | Neurology | Nutrition | OSCE | Obstetrics Gynaecology | Oncology | Ophthalmology | Oral Medicine and Dentistry | Paediatrics | Palliative | Pathology | Pharmacology | Physiology | Procedures | Psychiatry | Radiology | Respiratory | Resuscitation | Rheumatology | Statistics and Research | Stroke | Surgery | Toxicology | Trauma and Orthopaedics | Twitter | Urology
Related Subjects: |Herpes Varicella-Zoster (Shingles) Infection |Herpes Viruses |Herpes Zoster Ophthalmicus (HZO) Shingles |MonkeyPox |Mumps |Measles |Rubella (German Measles) |Epstein-Barr Virus infection |Cytomegalovirus (CMV) infections |CMV retinitis infections |Toxoplasmosis |Respiratory Failure
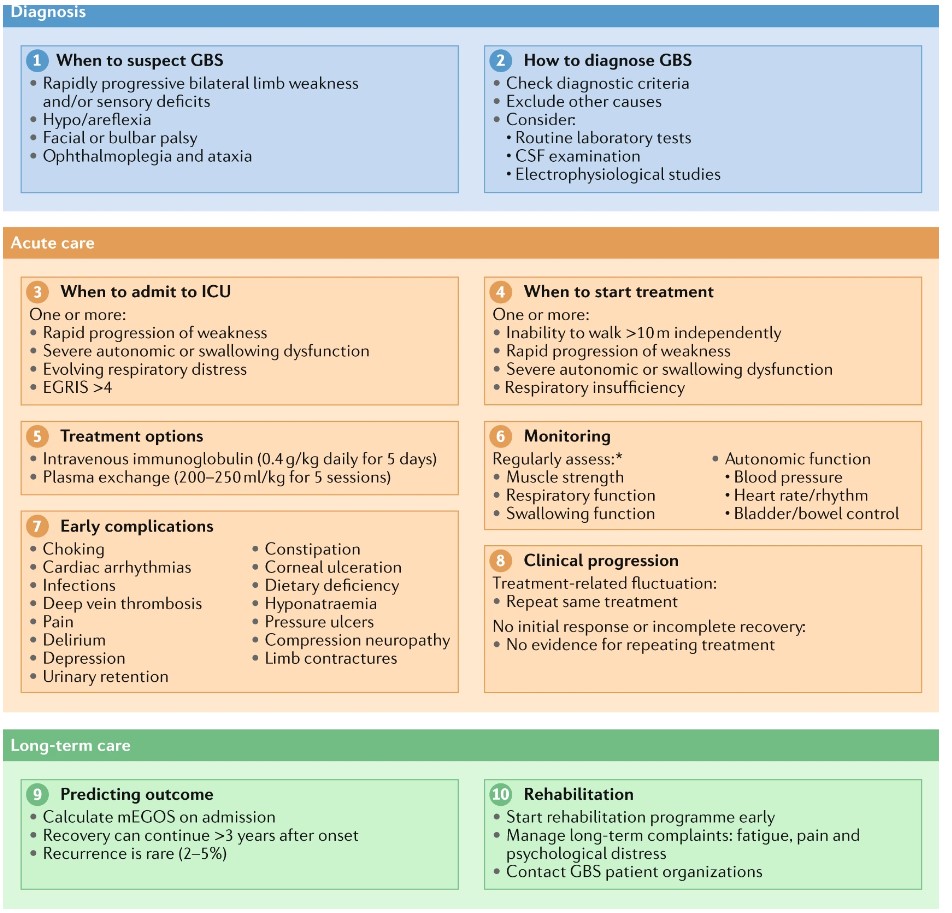
Respiratory function should be monitored in all patients as respiratory failure can occur without symptoms of dyspnoea. About 20% of patients with GBS develop respiratory failure and require mechanical ventilation. The bedside measure of respiratory muscle function is Forced Vital Capacity and a value < 1.5 Litre should suggest ITU admission. Cochrane review suggested that IVIG given within 2 weeks of the onset was as efficacious as plasma exchange, and more likely to be completed.
| Initial Management GBS |
|---|
|
About
- Acute onset over days of weakness with areflexia.
- Rare but potentially lethal with respiratory failure in some cases
- Early diagnosis and management is important
- Also known as Acute inflammatory demyelinating polyneuropathy
Aetiology
- Some are due to auto reactive T cells responding to an autoantigen
- Campylobacter jejuni, CMV, HIV, HEV, EBV, Mycoplasma, Zika virus, Lyme disease
- Multifocal demyelination, raised CSF protein which may be normal in the early stages.
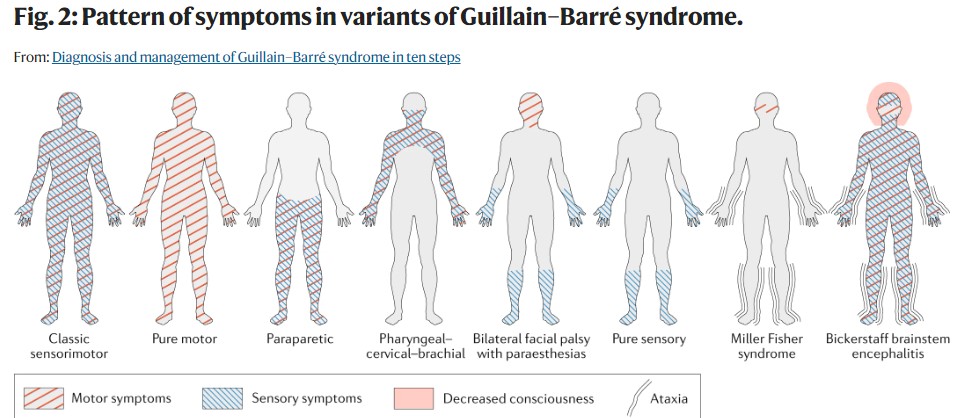
Different forms
- 90% AIDP: Acute inflammatory demyelinating polyradiculoneuropathy - various antibodies
- 5% AMAN: Acute motor (+/- sensory) axonal neuropathy - Anti GD1a (Bad prognosis with Campylobacter positive)
- 5% Miller-Fisher syndrome - ophthalmoplegia + ataxia + areflexia - anti GQ1b (Good prognosis)
- 1% AMSAN Acute Motor sensory neuropathy
Clinical
- Acute-onset ascending sensorimotor neuropathy
- Rapidly progressive bilateral weakness of the legs and/or arms,
- Dysautonomia: BP or heart rate instability, pupillary dysfunction
- Dysautonomia: bowel or bladder dysfunction
- Proximal weakness comes on over hours/days usually at worst by 14 days
- Moves from legs to trunk to chest and arms and head
- Isolated cranial nerve dysfunction can precede the onset of weakness
- Tingling in hands and feet and then difficulty rising from a chair
- Some experience severe back pain may be muscular, radicular or neuropathic
- Respiratory and swallowing weakness
- Distal Sensory loss may be present
- Areflexia -Tendon reflexes are lost as in keeping with the LMN signs
- Autonomic problems can occur - hypertension, arrhythmias
- Papilloedema due to high CSF protein
 >
>
Investigations
- FBC, U&E to check K+ Porphyrins
- ECG - arrhythmias - tachycardias and bradycardias
- Classically CSF protein is markedly raised 1-3 g by the second week but the WCC and Glucose levels remain normal. An early CSF protein may be normal.
- Nerve conduction studies may show demyelination which starts proximally. There is slowed conduction and focal conduction block. Absent F waves. May show axonal degeneration in AMAN. However, can be normal in early cases.
- Antibody measurements rarely useful except prognostically e.g. GD1a
Differential
- Acute spinal cord disease with flaccid weakness
- Acute intermittent porphyria
- Myasthenia gravis
- Botulism - progressive weakness with no sensory symptoms with normal CSF
- Tick paralysis, Diphtheria, Poliomyelitis, Porphyria
Features supporting diagnosis
- Progression over days, up to 4wks
- Near symmetrical symptoms.
- Sensory symptoms/signs only mild
- CNS involvement (eg bilateral facial weakness)
- Recovery starts 2wks after the period of progression has finished
- Autonomic dysfunction
- Absence of fever at onset
- CSF protein ↑ with CSF WCC <10.106/L
- Typical electrophysiological tests
Assess for ITU/Ventilation if breathlessness at rest or during talking, inability to count to 15 in a single breath, use of accessory respiratory muscles, increased respiratory or heart rate, vital capacity <15–20 ml/kg or <1 l, or abnormal arterial blood gas or pulse oximetry measurements. Risk factors for prolonged mechanical ventilation include the inability to lift the arms from the bed at 1 week after intubation, and an axonal subtype or unexcitable nerves in electrophysiological studies. Early tracheostomy should be considered in patients who have these risk factors.
Indication for ITU and/or Intubation
- Respiratory distress with imminent respiratory insufficiency
- FVC <15-20 mL/kg
- Maximal inspiratory pressure > -30 cmH₂O (negative inspiratory force)
- Maximal expiratory pressure is <40 cmH₂O
- Hypoxia despite increased FiO₂
- Severe swallowing dysfunction or diminished cough reflex
- Severe autonomic cardiovascular dysfunction
- Abnormal arterial blood gas or pulse oximetry measurements.
Management
- ABC. Manage in HDU if any respiratory concerns. ECG and BP monitoring for autonomic difficulties. Beware need for respiratory support and autonomic problems which can lead to dysrhythmia.
- Tracheal suction can cause hypotension due to autonomic instability. Monitor FVC for respiratory muscle weakness - intubation may be needed. Close liaison with ITU and outreach teams should be maintained.
- Immune Modulation Treatments: Start in patients who are unable to walk independently for 10 m. Evidence on treatment efficacy in patients who can still walk independently is limited. Also consider if rapidly progressive weakness or other severe symptoms such as autonomic dysfunction, bulbar failure or respiratory insufficiency.
- High dose IV immunoglobulins are given within the first 2 weeks which has been shown to improve duration and severity. IgA deficiency must be screened for before treatment commenced or else severe allergic reactions may occur. Usually, 0.4 g/kg/day for 5 days is given. Expensive.
- Plasma exchange started within 4 week. Plasma exchange (PLEX) is also effective but IVIG tends to be more easily given. PLEX preferred if IgA deficiency or renal failure. Needs central venous access. Four plasma exchanges for severe GBS. Two when mild. In some cases where the response is poor, a second course may be considered or plasma exchange tried.
- Steroids have been shown to be of no value in GBS. Plasma exchange followed by IVIg is no more effective than treatment alone.
- Pregnancy: Neither IVIg nor plasma exchange is contraindicated during pregnancy. However, as plasma exchange requires additional considerations and monitoring, IVIg might be preferred
- There is a high risk of VTE and so Heparin/LMWH must be given or IPC stockings.
- Patients will often need ongoing rehabilitation over weeks and months involving physiotherapy and occupational therapy
- Speech and language therapy if bulbar weakness to assess swallow - NG feeding in the interim and PEG if a delayed return of bulbar function
- Neuropathic pain is not uncommon - Carbamazepine and Gabapentin and opiates as required. Amitriptyline should be avoided as it can theoretically cause arrhythmias.
- Effective use of laxatives to avoid constipation which may well result from opiates and immobility
- Outcome
- Clinical improvement is usually most extensive in the first year after disease onset and can continue for >5 years.
- 85% may have a good recovery, others are left with a degree of disability
- Usually monophasic but can recur and may even become progressive resembling CIDP
- Worse outcome post diarrhoea, older patient, rapid onset, muscle wasting
Complications
- Bulbar palsy: Choking, Dietary deficiency
- Cardiac arrhythmias
- Limited communication: Delirium, Depression, Pain and tactile allodynia
- Bulbar and facial palsy: Corneal ulceration, immobility, bladder dysfunction, mechanical ventilation
- Immobility: Urinary retention, Constipation, Pressure ulcers, Hospital-acquired infections (e.g., pneumonia, sepsis or urinary tract infection), Compression neuropathy, Limb contractures and ossifications
- Hyponatraemia