Makindo Medical Notes.com |
|
|---|---|
| Download all this content in the Apps now Android App and Apple iPhone/Pad App | |
| MEDICAL DISCLAIMER:The contents are under continuing development and improvements and despite all efforts may contain errors of omission or fact. This is not to be used for the assessment, diagnosis or management of patients. It should not be regarded as medical advice by healthcare workers or laypeople. It is for educational purposes only. Please adhere to your local protocols. Use the BNF for drug information. If you are unwell please seek urgent healthcare advice. If you do not accept this then please do not use the website. Makindo Ltd | |
Resuscitation - Basic Life Support ABCDE
-
| About | Anaesthetics and Critical Care | Anatomy | Biochemistry | Cardiology | Clinical Cases | CompSci | Crib | Dermatology | Differentials | Drugs | ENT | Electrocardiogram | Embryology | Emergency Medicine | Endocrinology | Ethics | Foundation Doctors | Gastroenterology | General Information | General Practice | Genetics | Geriatric Medicine | Guidelines | Haematology | Hepatology | Immunology | Infectious Diseases | Infographic | Investigations | Lists | Microbiology | Miscellaneous | Nephrology | Neuroanatomy | Neurology | Nutrition | OSCE | Obstetrics Gynaecology | Oncology | Ophthalmology | Oral Medicine and Dentistry | Paediatrics | Palliative | Pathology | Pharmacology | Physiology | Procedures | Psychiatry | Radiology | Respiratory | Resuscitation | Rheumatology | Statistics and Research | Stroke | Surgery | Toxicology | Trauma and Orthopaedics | Twitter | Urology
Related Subjects: |Adrenaline/Epinephrine |Atropine |Adult Resus:Acute Anaphylaxis |Adult Resus:Basic Life Support |Adult Resus: Advanced Life Support |Adult Resus: Obstetric Cardiac Arrest |Newborn/Child Resus: All |Acute Hypotension |Cardiogenic shock |Distributive Shock |Hypovolaemic or Haemorrhagic Shock |Obstructive Shock |Septic Shock and Sepsis |Shock (General Assessment) |Toxic Shock Syndrome |Resus:Bradycardia |Resus:Tachycardia |Resus:Hyperkalaemia |Resus:Post Resuscitation Algorithm |Resus:Acute Severe Asthma |Resus:Acute Haemorrhage
Unresponsive then shout for help and open airway. Still not breathing normally then call 999 and start with 30 chest compressions. 2 rescue breaths and then 30 compressions.
Basic Algorithm
| Immediate Assessment |
|---|
|
Assessment
- Approach cautiously. Ensure a safe environment for you and the patient and bystanders. Beware electrical, chemical, water, roadside hazards. Check the victim for a response.
- Gently shake his shoulders and ask loudly, "are you all right". If there is a response leave in the position in which you find him provided there is no further danger.
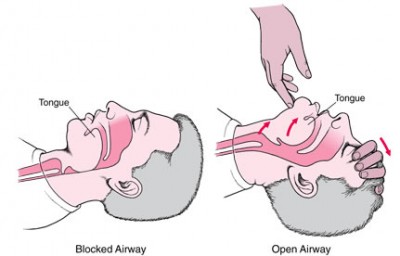
- Try to find out what is wrong with the individual and get help if needed. Reassess the patient regularly. If there is no satisfactory response then ABC: Perform head tilt, chin-lift manoeuvre.
AIRWAY
- If (s)he does not respond then shout for help. Turn the victim onto their back and then open the airway by placing two fingers under the chin and lifting.
- One can also place fingers behind the mandible at the angle of the jaw and lift forwards and upwards. Check the mouth for debris with a finger sweep.
- False teeth need not be removed unless they are obstructing the airway or loose or poorly fitting.
Head tilt, chin lift, jaw thrust : Caution if neck injury
Inserting an oral airway

| Signs of Airway Obstruction |
|---|
|
| Management |
|
BREATHING
- Keeping the airway open, look, listen, and feel for normal breathing. Look for chest movement, Listen at the victim's mouth for breath sounds. Feel for air on your cheek. In the first few minutes after cardiac arrest, a victim may be barely breathing or taking infrequent, noisy, gasps. This is often termed agonal breathing and must not be confused with normal breathing. Look, listen, and feel for no more than 10 s to determine if the victim is breathing normally.
- If you have any doubt whether breathing is normal, act as if it is not normal. If he is breathing normally place in the recovery position and summon help from the ambulance service by mobile phone. If this is not possible, send a bystander. Leave the victim only if no other way of obtaining help is possible.
- Continue to assess that breathing remains normal. If there is any doubt about the presence of normal breathing, start CPR. If he is not breathing normally. Ask someone to call for an ambulance and bring an AED if available. If you are on your own, use your mobile phone to call an ambulance. Leave the victim only when no other option exists for getting help.
| Causes of Breathlessness |
|---|
|
CIRCULATION
- Feel for a major pulse - carotid or femoral. If none found then commence CPR. Start chest compression as follows: Kneel by the side of the victim and place the heel of one hand in the centre of the victim's chest on the lower half of the sternum.
- Place the heel of your other hand on top of the first hand and interlock the fingers of your hands and ensure that pressure is not applied over the victim's ribs. Do not apply any pressure over the upper abdomen or the bottom end of the sternum.
- Position yourself vertically above the victim's chest and, with your arms straight, press down on the sternum 5 - 6 cm. After each compression, release all the pressure on the chest without losing contact between your hands and the sternum. Repeat at a rate of 100 - 120 /min. Compression and release should take an equal amount of time.
Combine chest compression with rescue breaths
- After 30 compressions open the airway again using head tilt and chin lift. Pinch the soft part of the victim's nose closed, using the index finger and thumb of your hand on his forehead.
- Allow his mouth to open, but maintain chin lift. Take a normal breath and place your lips around his mouth, making sure that you have a good seal.
- Blow steadily into his mouth whilst watching for his chest to rise; take about one second to make his chest rise as in normal breathing; this is an effective rescue breath.
- Maintaining head tilt and chin lift, take your mouth away from the victim and watch for his chest to fall as air comes out.
- Take another normal breath and blow into the victim's mouth once more to give a total of two effective rescue breaths. The two breaths should not take more than 5 s. Then return your hands without delay to the correct position on the sternum and give a further 30 chest compressions.
- Continue with chest compressions and rescue breaths in a ratio of 30:2. Stop to recheck the victim only if he starts to show signs of regaining consciousness, such as coughing, opening his eyes, speaking, or moving purposefully AND starts to breathe normally; otherwise do not interrupt resuscitation.
- If the initial rescue breath of each sequence does not make the chest rise as in normal breathing, then, before your next attempt:
- Check the victim's mouth and remove any visible obstruction.
- Recheck that there is adequate head tilt and chin lift.
- Do not attempt more than two breaths each time before returning to chest compressions.
- If there is more than one rescuer present, another should take over CPR about every 1-2 min to prevent fatigue.
- Ensure the minimum of delay during the changeover of rescuers, and do not interrupt chest compressions.
Compression-only CPR
If you are not trained to or are unwilling to give rescue breaths, give chest compressions only. If chest compressions only are given, these should be continuous at a rate of 100 - 120 /min. Stop to recheck the victim only if he starts to show signs of regaining consciousness, such as coughing, opening his eyes, speaking, or moving purposefully AND starts to breathe normally; otherwise do not interrupt resuscitation. Continue resuscitation until qualified help arrives and takes over or the victim starts to show signs of regaining consciousness, such as coughing, opening his eyes, speaking, or moving purposefully AND starts to breathe normally, OR you become exhausted.
| Causes of Compromised Circulation |
|---|
|
| Signs of Compromised Circulation |
|---|
|
Disability (D) Assess if patient is
- Awake (A): spontaneously awake responds environment.
- Responding to voice (V): opens eyes or responds only to speech other than sleeping
- Responding to pressure (P): responds only to pressure/painful stimuli. Examples of painful stimuli include the 'trapezius squeeze'.
- Unresponsive (U): no response to voice or pressure
An assessment of neurological status. The level of consciousness can be done using the AVPU system. If you're concerned about the patient's level of consciousness, then use a more in-depth assessment, such as the Glasgow Coma Scale (GCS). Always exclude hypoglycaemia by quickly testing. If delayed then give IV Glucose or IM Glucagon.Also, consider opiate overdose with small pupils. Even codeine enough can cause coma. Give naloxone if suspected. Get expert help as to cause and next steps. Unconscious patients whose airways are not protected should be nursed in the lateral position. Give oxygen. In those with a GCS< 9 who may not airway protect needs an anaesthetic review of airways management and need or intubation. The question may well be the need for a CT head to look for structural problems. Talk to your senior.
Exposure (E)
- Check top to toe. Look for presence of rashes, bruises, swelling, bleeding or any excessive losses from drains. Respect the patient's dignity at all times and minimise heat loss.