Makindo Medical Notes.com |
|
|---|---|
| Download all this content in the Apps now Android App and Apple iPhone/Pad App | |
| MEDICAL DISCLAIMER:The contents are under continuing development and improvements and despite all efforts may contain errors of omission or fact. This is not to be used for the assessment, diagnosis or management of patients. It should not be regarded as medical advice by healthcare workers or laypeople. It is for educational purposes only. Please adhere to your local protocols. Use the BNF for drug information. If you are unwell please seek urgent healthcare advice. If you do not accept this then please do not use the website. Makindo Ltd | |
Broad Complex Tachycardia
-
| About | Anaesthetics and Critical Care | Anatomy | Biochemistry | Cardiology | Clinical Cases | CompSci | Crib | Dermatology | Differentials | Drugs | ENT | Electrocardiogram | Embryology | Emergency Medicine | Endocrinology | Ethics | Foundation Doctors | Gastroenterology | General Information | General Practice | Genetics | Geriatric Medicine | Guidelines | Haematology | Hepatology | Immunology | Infectious Diseases | Infographic | Investigations | Lists | Microbiology | Miscellaneous | Nephrology | Neuroanatomy | Neurology | Nutrition | OSCE | Obstetrics Gynaecology | Oncology | Ophthalmology | Oral Medicine and Dentistry | Paediatrics | Palliative | Pathology | Pharmacology | Physiology | Procedures | Psychiatry | Radiology | Respiratory | Resuscitation | Rheumatology | Statistics and Research | Stroke | Surgery | Toxicology | Trauma and Orthopaedics | Twitter | Urology
Related Subjects: |Classical Ventricular Tachycardia |Idiopathic Ventricular Tachycardia |Ventricular Fibrillation |Resuscitation - Adult Tachycardia Algorithm |Resuscitation - Advanced Life Support |Atrial Flutter |Atrial Fibrillation |Wolff-Parkinson White syndrome (WPW) |Supraventricular Tachycardia (SVT)
Treat any regular broad complex tachycardia as VT rather than an SVT with aberrant conduction. Look for AV dissociation signs - irregular notching of the QRS complex, capture beats and fusion beats. A past history of ischaemic heart disease is associated with a >95% chance that broad complex tachycardia is VT.
About
- Wide or Broad complex QRS is > 3 small squares wide or 120 ms
- Definition of VT is a wide complex regular tachycardia (rate > 120/min)
- Treat as Ventricular tachycardia. Treat the patient as potentially peri-arrest
Broad complex Tachycardia can be divided on basis of regularity
- Regular
- Ventricular Tachycardia
- SVT with aberrant conduction
- Idioventricular rhythm - seen post MI but rate usually < 120/min
- Atrial flutter with aberrant conduction
- Atrial flutter/SVT with WPW
- Irregular
- Atrial fibrillation with aberrant conduction
- Pre excited AF (WPW) - delta wave and irregularly irregular
- Torsade de pointes
Clinical
- Chest pain and angina (IHD is the commonest cause of VT)
- Variable intensity of S1 in a regular tachycardia suggests AV dissociation causing variable filling of the ventricles from the atria.
- Hypotensive/Cardiogenic shock as output falls
- Check for a cardiac history of IHD makes VT more likely
Investigations
- Check FBC, U&E, Mg and Troponin
- Echocardiogram at first opportunity to determine LV
- If the patient is stable always get a 12 lead ECG
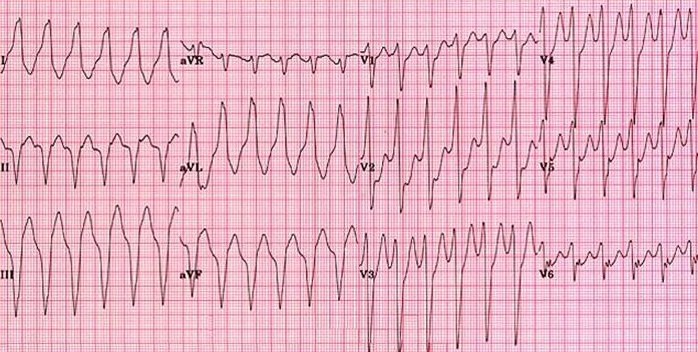
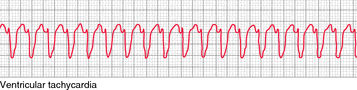 VT
VT
ECG findings that favour VT (for post hoc analysis - treat as VT)
- Fusion (hybrid narrow/wide complex) beats : simultaneous activation of the ventricles from a focus of arrhythmia and from the atria via the AV node at the same time. Look like a cross between the standard VT complex and the patient’s normal complexes in sinus rhythm.
- Capture (narrow) beats: occasionally the atria ‘capture’ a normal complex in the midst of a tachycardia.
- May see evidence of both atrial and ventricular activity. If there is no constant relationship between the P waves (if seen) and the QRS complexes, it suggests a ventricular origin and this is called atrioventricular dissociation.
- History of IHD or structural heart disease
- Absence of RS wave on chest leads
- RBBB pattern > 0.14 secs or LBBB pattern > 0.16 secs
- Extreme Left Axis Deviation
- Extreme R to R regularity
- A very broad QRS (>0.14 s)
- A bifid, upright QRS with a taller first peak in V1
- A deep S wave in V6
- Concordant (same polarity) QRS direction in all chest leads (V1–V6)
- No response to adenosine
Classical VT is by far the most common cause of wide complex regular tachycardia, and there is no perfectly reliable way to distinguish classic VT with all its dangers from idiopathic VT or SVT with aberrancy on the surface 12-lead ECG. Treat as Classical VT - follow Adult tachycardia algorithm above
Management
- ABC, Call Cardiac arrest if unresponsive and follow cardiac arrest protocol
- DC countershock for any tachyarrhythmia with haemodynamic compromise
- Adenosine can be tried and will terminate SVT or Right ventricular outflow tract VT Adenosine may also show flutter waves.
- See Adult Tachycardia Algorithm linked above