Makindo Medical Notes.com |
|
|---|---|
| Download all this content in the Apps now Android App and Apple iPhone/Pad App | |
| MEDICAL DISCLAIMER:The contents are under continuing development and improvements and despite all efforts may contain errors of omission or fact. This is not to be used for the assessment, diagnosis or management of patients. It should not be regarded as medical advice by healthcare workers or laypeople. It is for educational purposes only. Please adhere to your local protocols. Use the BNF for drug information. If you are unwell please seek urgent healthcare advice. If you do not accept this then please do not use the website. Makindo Ltd | |
Wolff-Parkinson White syndrome (WPW) AVRT
-
| About | Anaesthetics and Critical Care | Anatomy | Biochemistry | Cardiology | Clinical Cases | CompSci | Crib | Dermatology | Differentials | Drugs | ENT | Electrocardiogram | Embryology | Emergency Medicine | Endocrinology | Ethics | Foundation Doctors | Gastroenterology | General Information | General Practice | Genetics | Geriatric Medicine | Guidelines | Haematology | Hepatology | Immunology | Infectious Diseases | Infographic | Investigations | Lists | Microbiology | Miscellaneous | Nephrology | Neuroanatomy | Neurology | Nutrition | OSCE | Obstetrics Gynaecology | Oncology | Ophthalmology | Oral Medicine and Dentistry | Paediatrics | Palliative | Pathology | Pharmacology | Physiology | Procedures | Psychiatry | Radiology | Respiratory | Resuscitation | Rheumatology | Statistics and Research | Stroke | Surgery | Toxicology | Trauma and Orthopaedics | Twitter | Urology
Related Subjects: |Wolff-Parkinson White syndrome (WPW) AVRT |Lown Ganong Levine Syndrome AVRT |Supraventricular Tachycardia (SVT) |Atrioventricular Nodal Reentrant Tachycardia AVNRT |Atrial Flutter |Atrial Fibrillation |Sinus Tachycardia |Sinus Arrhythmia |Multifocal Atrial Tachycardia |Resuscitation - Adult Tachycardia Algorithm
WPW syndrome is caused by an accessory pathway known as the Bundle of Kent. This pathway bypasses the normal electrical conduction system of the heart, which typically prevents the ventricles from being prematurely activated. As a result, this can lead to a reentrant tachycardia.
About
- Abnormal electrical connection between atrium and ventricle (e.g. bundle of Kent)
- This allows quick conduction from the atria to the ventricles bypassing the AV node.
- Ventricles are depolarized earlier than they would be and this is called pre-excitation.
Causes
- Normal conduction passes anterogradely through the AV node with no retrograde conduction.
- The bypass tract can conduct both directions depending on its characteristics.
- This can lead to an Atrioventricular reentrant tachycardia which may pass anterogradely or retrogradely through the AV node and accessory pathway.
- In AF the bypass tract can conduct unhindered to the ventricles with a risk of VF
Associations
- Septum secundum ASD
- Ebstein anomaly of tricuspid valve
- Hypertrophic cardiomyopathy
- Mitral valve prolapse
Clinical
- Often asymptomatic all lifelong despite ECG changes.
- Palpitations, Syncope, Presyncope.
- Very rarely sudden cardiac death possibly due to AF down accessory pathway
ECG Findings
- Resting ECG
- A concealed pathway: ECG is normal between arrhythmias no delta wave
- A manifest pathway: ECG: Short PR and slurred delta wave. May be an RSR pattern in V1 with Type A however there are several different types depending on location of accessory pathway.
- Arrhythmias
- Atrioventricular reentrant tachycardia (AVRT): Narrow complex with ressntrant pathway involving accessory pathway
- AF conducted to Ventricle across accessory pathway: irregularly irregular + delta wave. Can degenerate to VF
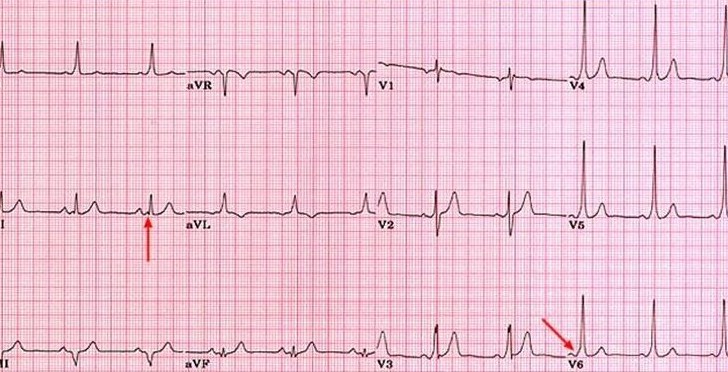
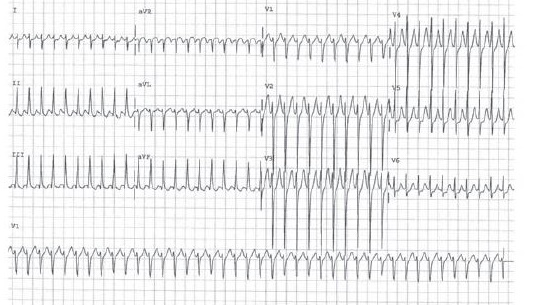
ECG showing Pre excitation
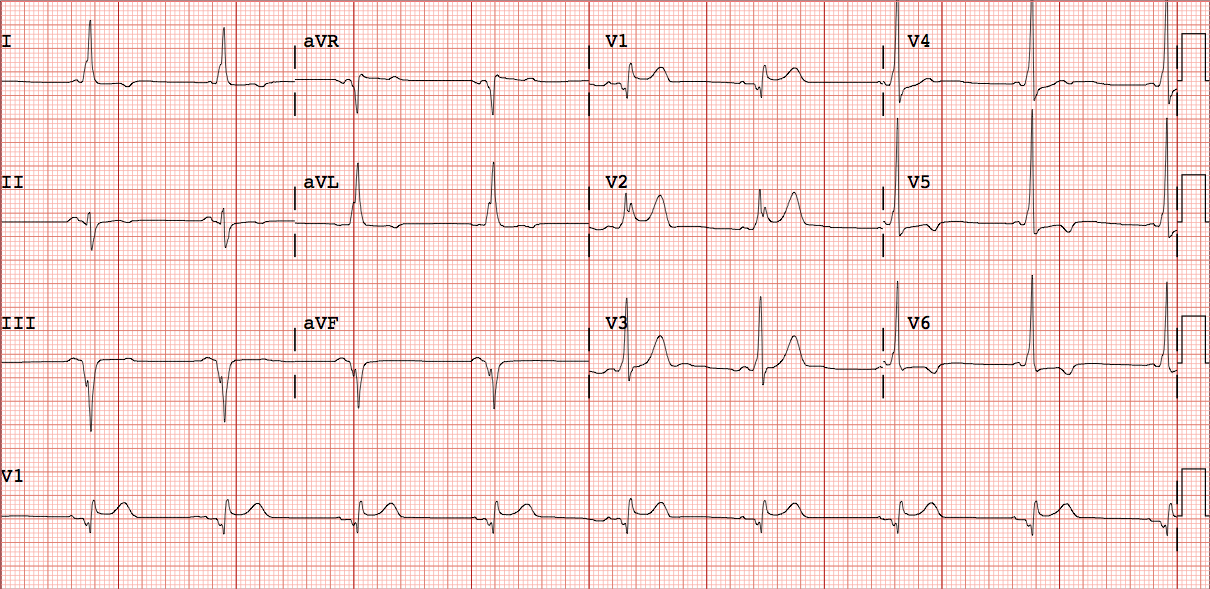
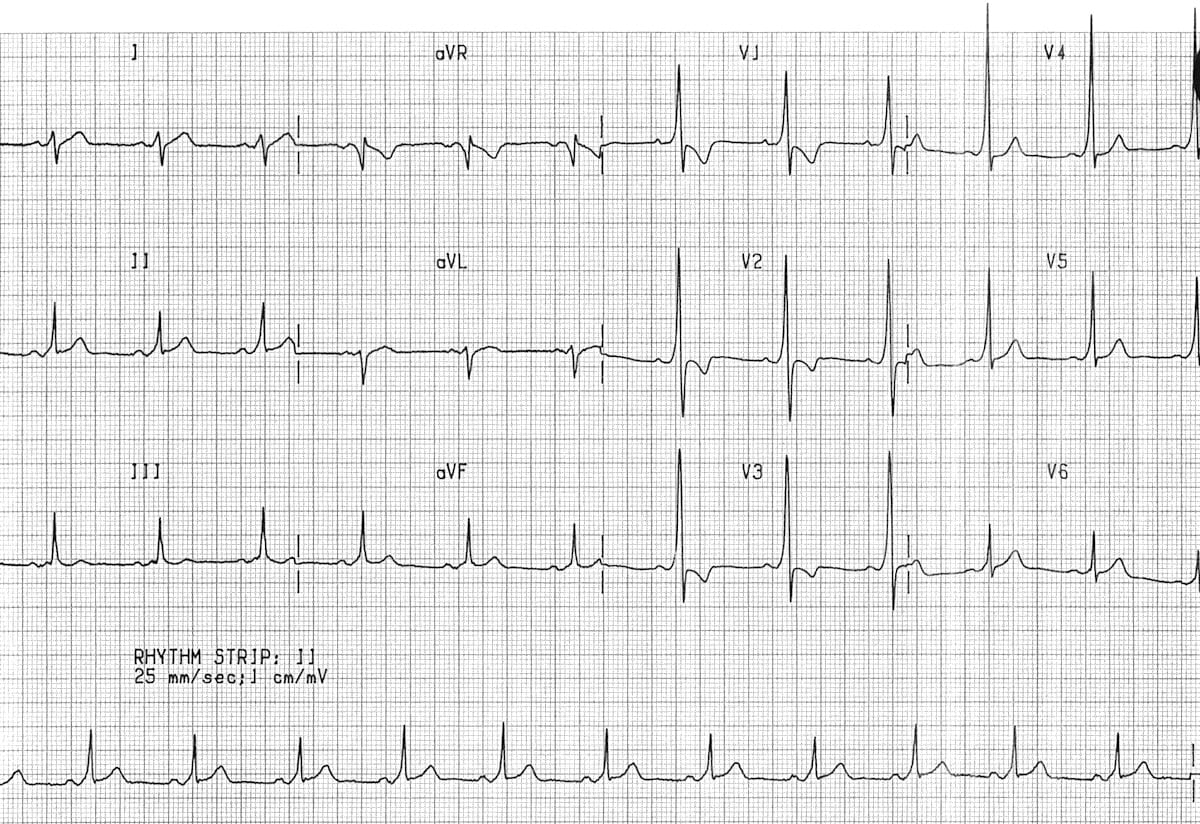
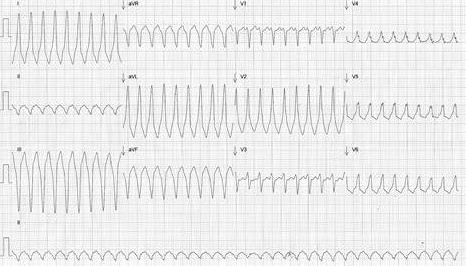
ECG showing AVNRT
Investigations
- FBC, U&E, TFT, CRP, ECG, CXR
- Echocardiogram or Cardiac MRI
- Electrophysiological studies
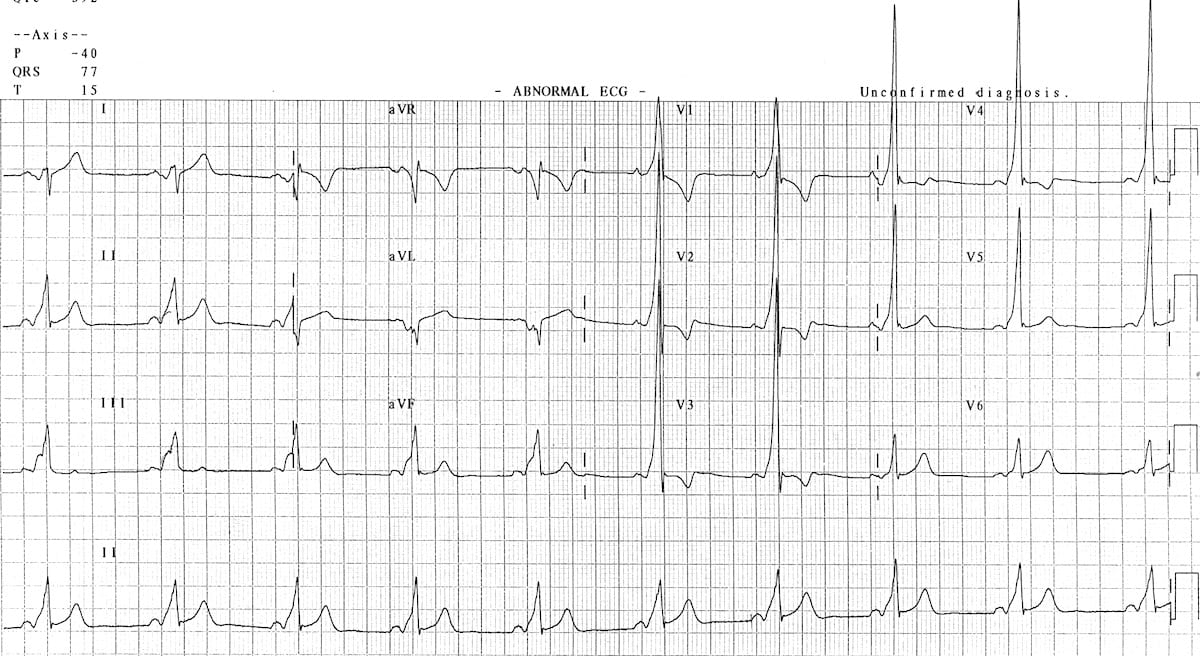
AF in a patient with ventricular pre-excitation
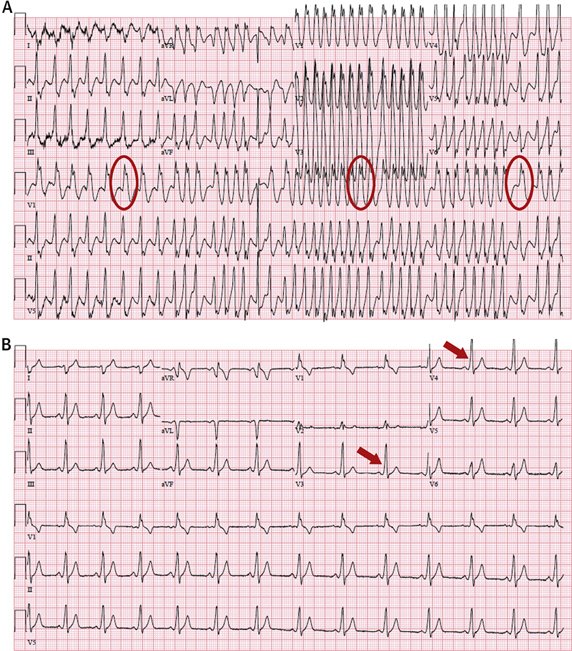
If suspect AF and Aberrant conduction down the accessory pathways then you must avoid Adenosine, Digoxin, Beta Blockers or Calcium Channel blockers
Acute Management: There are two scenarios that have specific management
- Regular Narrow Complex Tachycardia AVRT SVT: Can be treated with Vagal Manoeuvres or if that fails then Adenosine or if unstable DC cardioversion which should terminate the SVT. See SVT topic for more options. The arrhythmia can be antidromic (going down the AV Node and then back via accessory pathway) or antidromic going the opposite direction.
- Pre-excited AF: May have known WPW. Wide complex irregular (? AF). AF + delta down accessory pathway vent rate 200+. If compromised DC shock. Suggest IV Procainamide, Ibutilide, Propafenone, Flecainide. (NEVER GIVE Dig/BB/CCB/Adenosine) Needs Cardio consult and Catheter ablation. Amiodarone not recommended
- Patients presenting with pre-excited AF once managed should be referred for definitive treatment which is radiofrequency catheter ablation of the accessory pathway, not only to eliminate symptoms of palpitations but also to eliminate the risk of sudden death. The accessory pathway responsible for pre-excited AF or supraventricular tachycardia can be eliminated in about 95% of patients with a low risk of complications (1%).
- Some Patients may well require a pacemaker after Radiofrequency ablation as 1% end up with CHB as the pathway ablated lies very close to the AV node