Makindo Medical Notes.com |
|
|---|---|
| Download all this content in the Apps now Android App and Apple iPhone/Pad App | |
| MEDICAL DISCLAIMER:The contents are under continuing development and improvements and despite all efforts may contain errors of omission or fact. This is not to be used for the assessment, diagnosis or management of patients. It should not be regarded as medical advice by healthcare workers or laypeople. It is for educational purposes only. Please adhere to your local protocols. Use the BNF for drug information. If you are unwell please seek urgent healthcare advice. If you do not accept this then please do not use the website. Makindo Ltd | |
Pericardial Effusion and Tamponade
-
| About | Anaesthetics and Critical Care | Anatomy | Biochemistry | Cardiology | Clinical Cases | CompSci | Crib | Dermatology | Differentials | Drugs | ENT | Electrocardiogram | Embryology | Emergency Medicine | Endocrinology | Ethics | Foundation Doctors | Gastroenterology | General Information | General Practice | Genetics | Geriatric Medicine | Guidelines | Haematology | Hepatology | Immunology | Infectious Diseases | Infographic | Investigations | Lists | Microbiology | Miscellaneous | Nephrology | Neuroanatomy | Neurology | Nutrition | OSCE | Obstetrics Gynaecology | Oncology | Ophthalmology | Oral Medicine and Dentistry | Paediatrics | Palliative | Pathology | Pharmacology | Physiology | Procedures | Psychiatry | Radiology | Respiratory | Resuscitation | Rheumatology | Statistics and Research | Stroke | Surgery | Toxicology | Trauma and Orthopaedics | Twitter | Urology
Related Subjects: |Assessing Breathlessness |Assessing Chest Pain |Pericardial Effusion and Tamponade |Constrictive Pericarditis |Colchicine |Chest X Ray Interpretation
Tuberculosis (TB) is the most frequent cause of pericardial diseases in the world and developing countries, where TB is endemic. In the case of tamponade and Cardiac arrest decompress the pericardium immediately. Point of care echocardiography supports the diagnosis. Perform resuscitative thoracotomy or ultrasound-guided pericardiocentesis
About
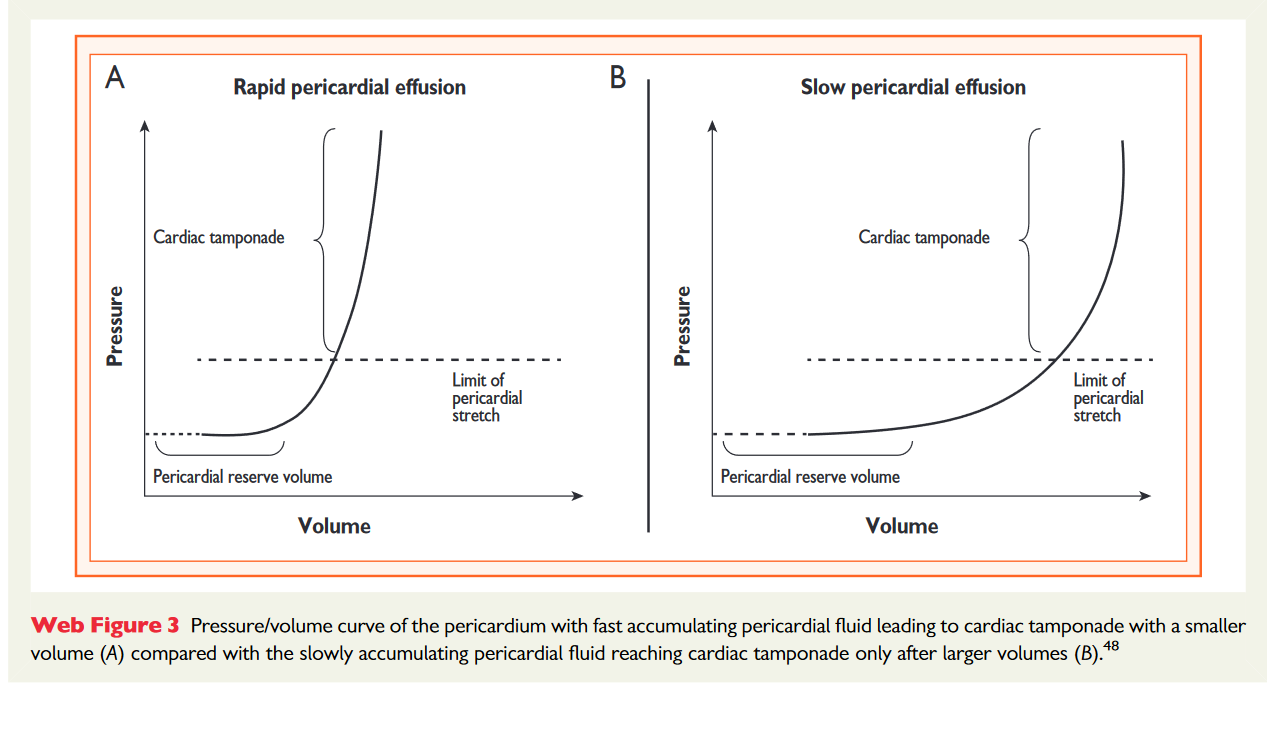
- Chronic fluid collection may be well tolerated, acute increases are usually not tolerated
- May simply be serous fluid from inflammation or malignancy but can also be blood
Aetiology
- Normally pericardial sac contains 10-50 ml of pericardial fluid that acts as a lubricant between the pericardial layers.
- Effusion from local inflammatory processes or failure of reabsorption.
- Pericardial sac fills with fluid and pressure exceeds filling pressure and cardiac output falls.
- Acute volumes of 200 mls can impair filling. Chronic volumes of 2 L can be well tolerated as pericardium stretches.
Classify Effusion
- Time based
- Acute or subacute < 3 months
- Chronic when lasting >3 months
- Distribution
- Circumferential
- Loculated)
- Haemodynamic impact
- None
- Cardiac tamponade
- Effusive-constrictive
- Composition
- Exudate
- Transudate
- Blood
- Rarely air or gas from bacterial infections
- Size
- Mild (<10 mm)
- Moderate (10-20 mm)
- Large (>20 mm)
Causes of Pericardial Effusion and Tamponade
- Trauma - bleeding or over anticoagulation
- Post-surgical or cardiology procedure
- Tuberculosis.
- Malignancy: breast, lung, melanoma, Hodgkin disease
- Aortic dissection with leaking into pericardial space
- Post MI with wall rupture day 3-10
- Connective tissue disease, Uraemia
Clinical (Effusion alone)
- Cough, weakness, fatigue, anorexia and palpitations
- Dyspnoea on exertion, orthopnea, PND, Sinus tachycardia
- Systemic: Underlying cause e.g. TB, malignancy
- Pericarditis type chest pain and malaise and fever
- Hoarseness (pressure on TLN), nausea (diaphragm), dysphagia ( oesophagus)
With pulsus paradoxus the pulse fades on inspiration
Clinical of Tamponade
- Breathlessness and distress
- Beck's triad
- Distended Jugular veins
- Arterial Hypotension
- Diminished heart sounds
- High JVP with absent Y descent. Cachexia ? TB ? Malignancy
- Pulsus paradoxus: SBP falls > 10 mmHg in inspiration
- Bronchial breath sounds may be heard in the left axilla or left base because of bronchial compression which leads to lower lung atelectasis. [Ewart's sign]
- Kussmaul's sign is not typically seen (it is seen in Constrictive pericarditis)
Investigations
- FBC: anaemia, CRP, ESR. U&E: renal failure is a cause
- CRP/ESR: infection, inflammatory or autoimmune disease. Cardiac tamponade without inflammatory signs is associated with a higher risk of a neoplastic aetiology
- TFT: hypothyroid with low T4 and high TSH
- Clotting: INR and coagulation screen
- ECG: Low voltage ECG, tachycardia and even electrical alternans. Exclude STEMI
- CXR: increased cardiothoracic ratio only occurs with pericardial effusions exceeding 300 ml. large globular heart caused by pericardial effusion or may even be normal
- Echocardiography: An effusion is seen and there is the diastolic collapse of the lower pressure right atria and ventricle. The right ventricle may be slit-like. Left atrial collapse may also be seen and is specific. Poor stroke volume. There is back pressure with a large dilated IVC commensurate with a fall in forward flow.
- CT and CMR provide a larger field of view, allowing the detection of loculated pericardial effusion and pericardial thickening and masses, as well as associated chest abnormalities
- Microscopy and culture: Send pericardial fluid for Gram stain, bacterial cultures, acid-fast bacilli stain and culture, PCR, Cytology, and carcinoembryonic antigen.
Large globular heart of Pericardial Effusion
Echo shows diastolic collapse of the RV
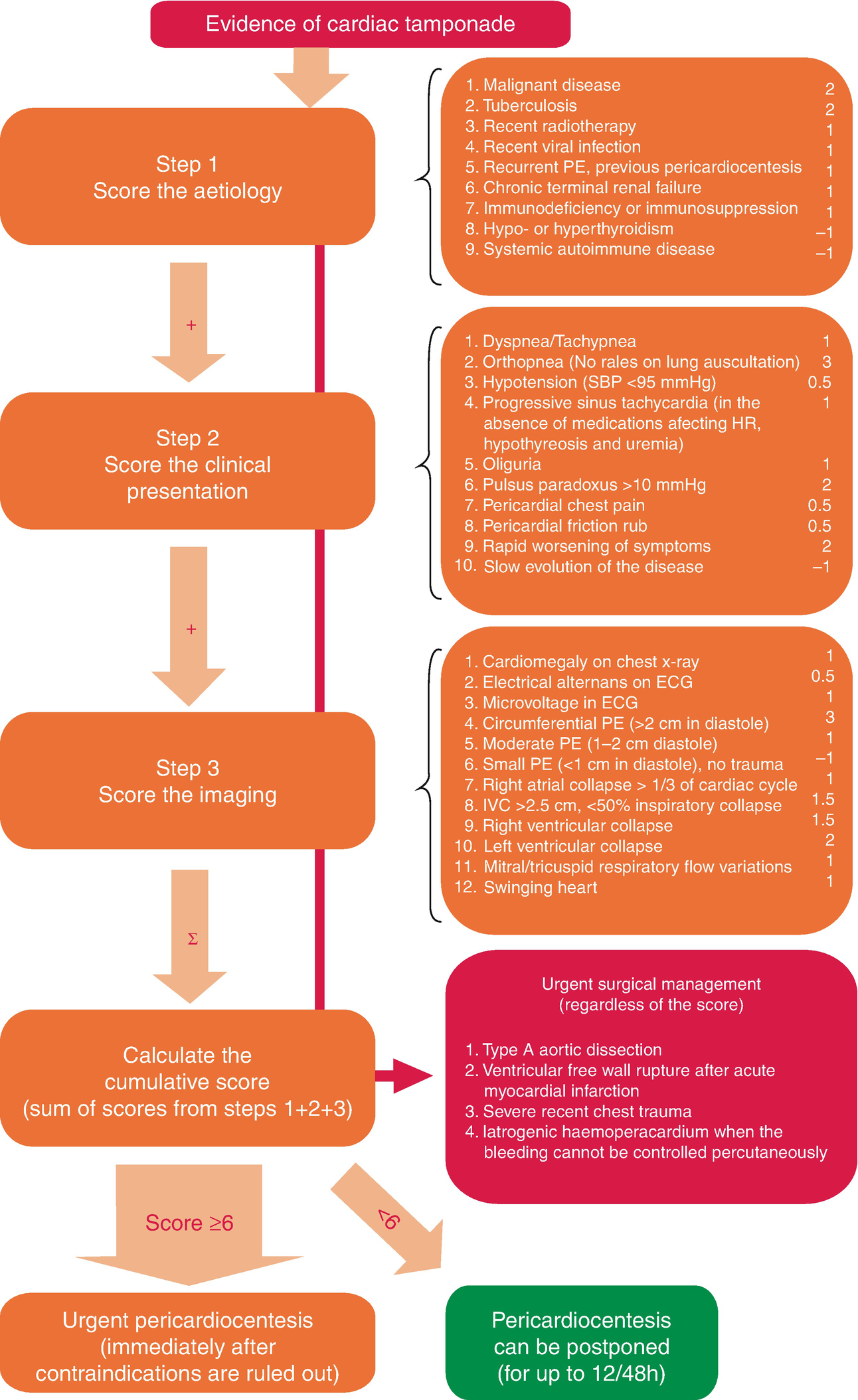
Algorithm for deciding need for Emergency Pericardiocentesis
Management
- ABC, IV fluids and volume expanders may be used carefully and initially but if compromised and in extremis or cardiac arrest then emergency treatment is needle pericardiocentesis to treat or prevent tamponade often leaving in a drain to avoid recollection of fluid and discussion and transfer to Cardiac Surgery for assessment for surgical treatment with pericardiectomy or fenestration to prevent re-accumulation may be indicated.
- Reverse any anticoagulation if there is any suspected bleeding into pericardial space suspected.
- If markers of inflammation are elevated, a trial of NSAIDs and/or Colchicine and/or low-dose corticosteroids may be tried if infection is excluded. A mild idiopathic effusion (<10 mm) is usually asymptomatic, generally has a good prognosis and does not require specific monitoring
- Conservative "wait and see" or masterly inactivity and monitor closely management may be reasonable if the patient is stable
- Emergency Pericardiocentesis: should be performed via the xiphisternal route, preferably under ultrasound guidance. A long needle is inserted 1 cm below the xiphisternum and angled to point towards the left shoulder (45 degrees). The ECG V lead is attached to the needle. Any damage to the myocardium shows up as ST elevation. The relief should be rapid and a fine catheter should be inserted for continuous drainage until the underlying condition is corrected. Definitive surgery is required if needle drainage is unsuccessful.
- If a recurrence is likely then pericardiectomy or less invasive options (i.e. pericardial window) should be considered whenever fluid reaccumulates, becomes loculated or biopsy material is required.
Pericardiocentesis is usually done under ultrasound guidance where possible. Here is a link to a youtube video