Makindo Medical Notes.com |
|
|---|---|
| Download all this content in the Apps now Android App and Apple iPhone/Pad App | |
| MEDICAL DISCLAIMER:The contents are under continuing development and improvements and despite all efforts may contain errors of omission or fact. This is not to be used for the assessment, diagnosis or management of patients. It should not be regarded as medical advice by healthcare workers or laypeople. It is for educational purposes only. Please adhere to your local protocols. Use the BNF for drug information. If you are unwell please seek urgent healthcare advice. If you do not accept this then please do not use the website. Makindo Ltd | |
Pulmonary Embolism
-
| About | Anaesthetics and Critical Care | Anatomy | Biochemistry | Cardiology | Clinical Cases | CompSci | Crib | Dermatology | Differentials | Drugs | ENT | Electrocardiogram | Embryology | Emergency Medicine | Endocrinology | Ethics | Foundation Doctors | Gastroenterology | General Information | General Practice | Genetics | Geriatric Medicine | Guidelines | Haematology | Hepatology | Immunology | Infectious Diseases | Infographic | Investigations | Lists | Microbiology | Miscellaneous | Nephrology | Neuroanatomy | Neurology | Nutrition | OSCE | Obstetrics Gynaecology | Oncology | Ophthalmology | Oral Medicine and Dentistry | Paediatrics | Palliative | Pathology | Pharmacology | Physiology | Procedures | Psychiatry | Radiology | Respiratory | Resuscitation | Rheumatology | Statistics and Research | Stroke | Surgery | Toxicology | Trauma and Orthopaedics | Twitter | Urology
Related Subjects: |Assessing Chest Pain |Assessing Breathlessness |Acute Coronary Syndrome (ACS) General |Aortic Dissection |Pulmonary Embolism |Acute Pericarditis |Diffuse Oesophageal Spasm |Gastro oesophageal reflux |Oesophageal Perforation Rupture |Pericardial Effusion_Tamponade |Pneumothorax |Tension Pneumothorax |Shingles |Deep Vein Thrombosis |DVT/PE in pregnancy |CTPA |Adrenaline/Epinephrine |Atropine |Adult Resus:Acute Anaphylaxis |Adult Resus:Basic Life Support |Adult Resus: Advanced Life Support |Adult Resus: Obstetric Cardiac Arrest |Newborn/Child Resus: All |Acute Hypotension |Cardiogenic shock |Distributive Shock |Hypovolaemic or Haemorrhagic Shock |Obstructive Shock |Resus:Post Resuscitation Algorithm |Resus:Acute Severe Asthma |Resus:Acute Haemorrhage
Pulmonary emboli should be prevented by early mobilisation and use of low dose LMWH in all patients at increased risk. Untreated mortality is 30% which falls to 8% with treatment
| Initial PE Management Summary |
|---|
|
About
- In hospitalized patients strategies to prevent VTE are vital
- Occurs in 15-20 patients per 1000 in hospital of which 2-5 are fatal
- Assess and document the Well's score
Risks for VTE
- Major trauma, surgery, lower-limb fractures
- Joint replacements, spinal cord injury
- Cancer especially pancreatic cancer, haematological malignancies, lung cancer, gastric cancer, and brain cancer
- Oestrogen-containing oral contraceptive agents are associated with an elevated VTE risk
- Combined oral contraceptives (containing both an oestrogen and a progestogen) are associated with an approximately 2-6-fold increase in VTE risk over baseline
- Severe inherited thrombophilia
- In post-menopausal women who receive hormone replacement therapy, the risk of VTE varies widely depending on the formulation used
- Infection is a common trigger for VTE
- Blood transfusion and erythropoiesis-stimulating agents are also associated with an increased risk of VTE
- Serious chronic medical conditions and central venous lines are considered likely triggers of PE
- Cigarette smoking, obesity, hypercholesterolaemia, hypertension, and diabetes mellitus
- Myocardial infarction and heart failure increase the risk of PE
- Protein C and S deficiencies
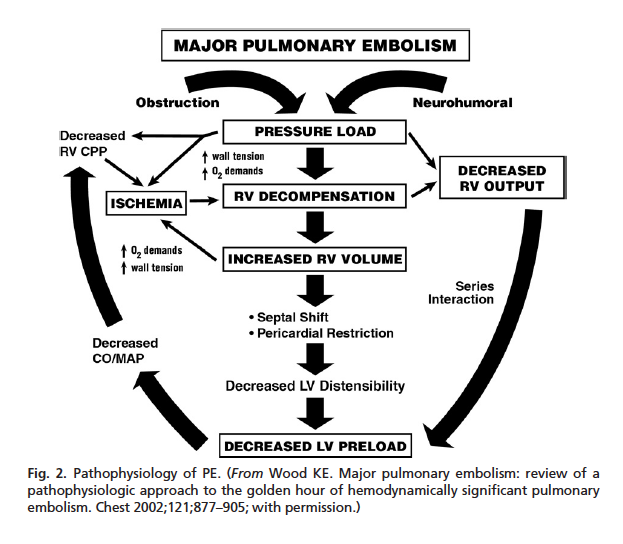
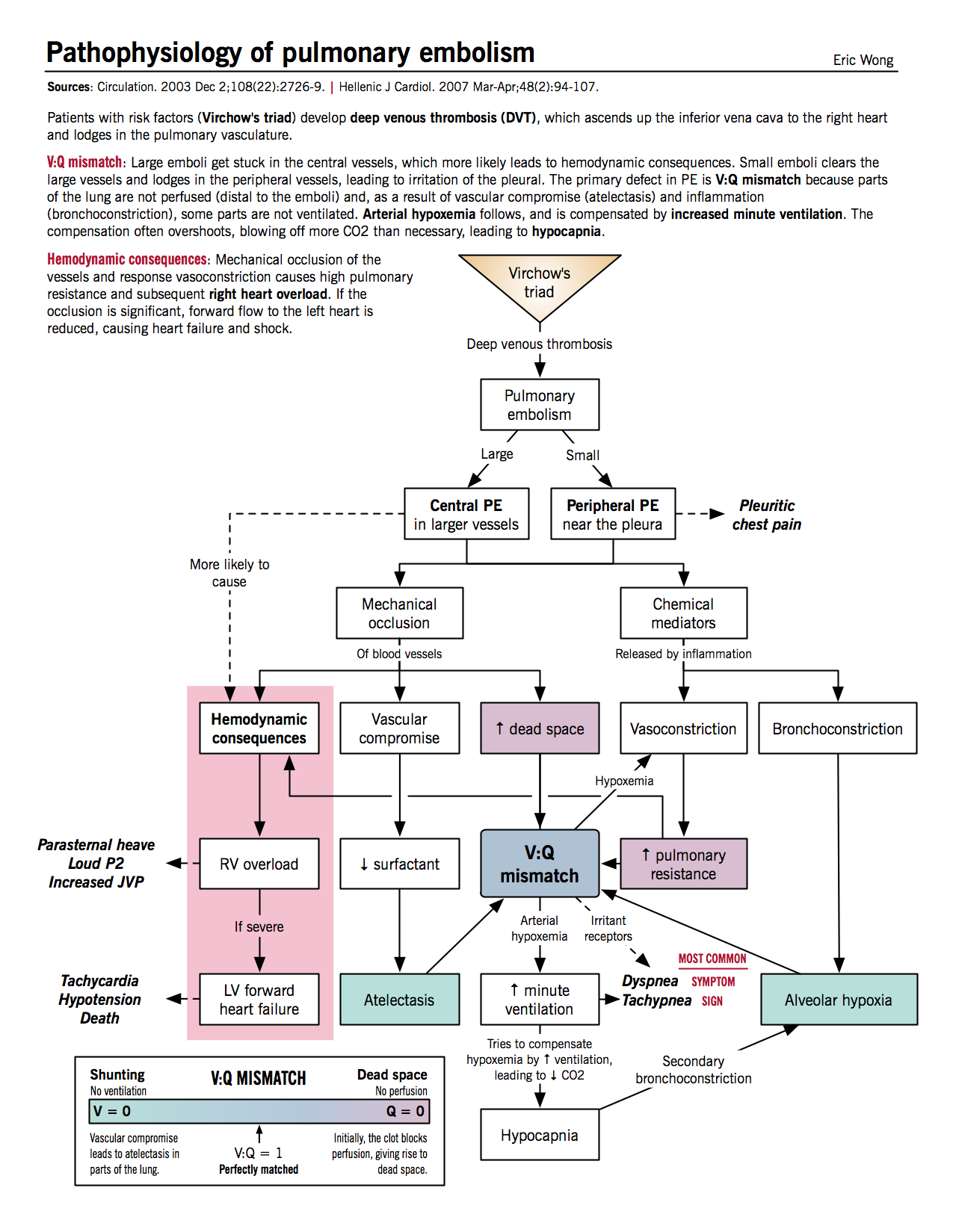
Pathophysiology
Clinical
- Assess BP, tachycardia, hypoxic, hypotensive, raised JVP. More comfortable flat. Clear lungs, Loud P2.
- Small sized emboli: Initially asymptomatic but overtime multiple recurrent thromboembolism leads to progressive breathlessness and ultimately cor pulmonale and pulmonary hypertension. Single small emboli may be subtle and non-specific e.g., causing confusion especially in the elderly.
- Medium sized embolism: Dyspnoea, possibly haemoptysis, pleuritic chest pain, pleural rub
- Large sized embolism: Usually when blood to more than two lobes is obstructed. There is acute right heart failure with marked dyspnoea, urge to defaecate (often collapse in the toilet), chest pain, tachycardia, raised JVP and loud P2 on auscultation. Hypotension.
- Massive sized embolism: Sudden cardiac death
- Paradoxical embolism: thrombus passes across a right to left shunt to the systemic circuit via the aorta and can cause stroke or infarction elsewhere - gut, limb, brain.
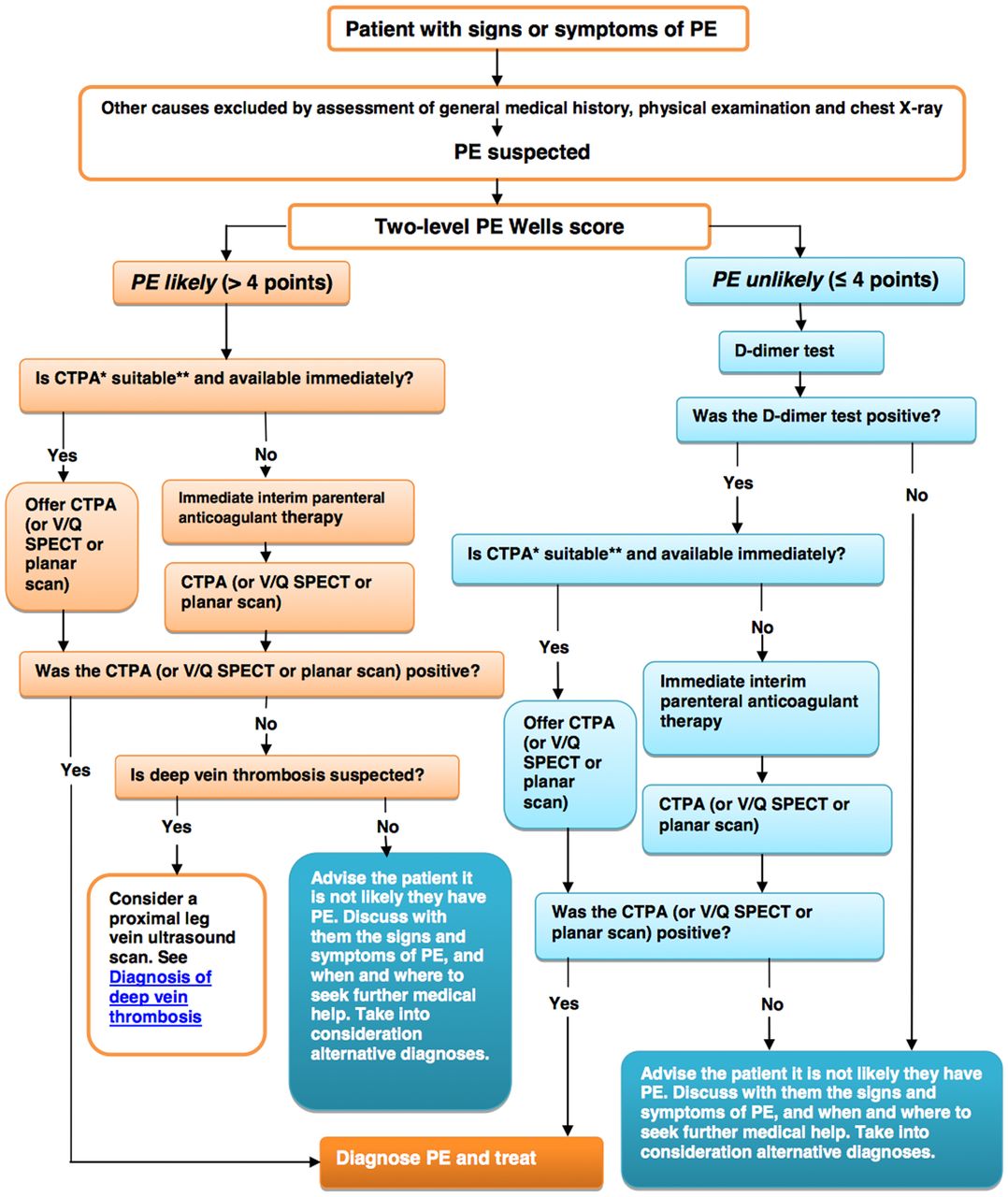
Well's score
- If score > 4 or more then perform CTPA and if positive treat
- If score < 4 then check dimer and CTPA if elevated and if positive treat
- Treat immediately if imaging delayed or high suspicion
| Well's Criteria for Pulmonary Embolism | |
|---|---|
| Clinical Signs and Symptoms of DVT ? | Yes +3 |
| PE is main diagnosis, or equally likely | Yes +3 |
| Heart Rate > 100 bpm? | Yes +1.5 |
| Immobilization at least 3 days, or Surgery in the Previous 4 weeks | Yes +1.5 |
| Previous, objectively diagnosed PE or DVT? | Yes +1.5 |
| Haemoptysis? | Yes +1 |
| Malignancy - Treatment within 6 mo, or palliative? | Yes +1 |
| Result | |
| Score > 6.0 - High (probability 59% based on pooled data) | |
| Score 2.0 to 6.0 - Moderate (probability 29% based on pooled data) | |
| Score < 2.0 - Low (probability 15% based on pooled data) | |
Investigations
- FBC and U&E, LFT's typically normal
- Arterial Blood gases: medium to large PE can cause low pO₂ and low/normal PCO₂ (Type 1 RF). In extremis may be acidotic.
- D-Dimer : D-dimer testing by ELISA 95% sensitive and by Latex agglutination 90% sensitivity. Only those patients classified as low or intermediate risk of PE should undergo quantitative D-dimer testing. The rest should have imaging either VQ or CTPA. If the D-dimer level is below your local lab cut off level then the diagnosis of PE can be excluded. The D-Dimer test is sensitive but not specific for PE. It is elevated in infections, malignancies and other processes. It is a degradation product of cross-linked fibrin.
- ECG findings : Commonest is sinus tachycardia. New atrial fibrillation. Others include S1Q3T3 pattern, right ventricular strain, new incomplete right bundle branch block. Alternatively, the ECG may be normal.
- CXR: a normal CXR is entirely compatible with a large PE. But other findings may include
- segmental collapse, pleural effusion, area of lung infarction
- raised hemidiaphragm, prominent pulmonary artery and a localised absence of vascular markings.
- Westermark sign with a focus of oligemia (hypovolemia) (leading to collapse of vessel) seen distal to a pulmonary embolism.
- Palla sign: enlargement of the descending pulmonary artery
- Troponin I/T: are elevated in 30-50% of large PEs
- Lactate: Elevated arterial plasma levels > 2 mmol/L predict PE-related complications,
- Echocardiogram: Right atria and Right ventricle dilated. Tricuspid regurgitation. Right heart strain. Pulmonary hypertension.
- USS legs: Occasionally PE is diagnosed indirectly by using Compression ultrasonography of legs to look for DVT. The treatment is the same. Not appropriate in the unstable patient needing urgent diagnosis. May be useful in pregnancy. The finding of a proximal thrombus in a patient suspected of DVT/PE is useful.
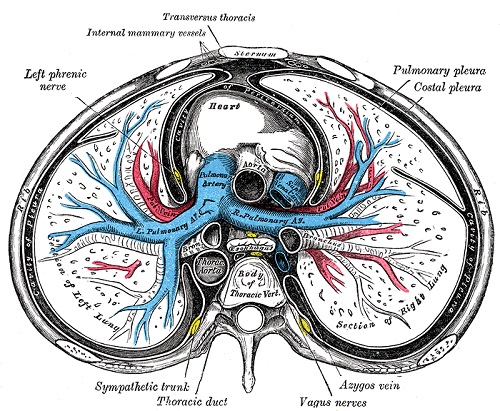
- Ventilation-perfusion scintigraphy (V/Q) scanning is used in many centres as the preferred initial imaging especially in pregnancy. However, of less use when the CXR is abnormal. A ventilation scan is done using inhaled radioactive xenon gas. Perfusion is measured using radiolabelled albumin macroaggregates. These are then compared to look for areas of mismatch. A PE can be identified by an area of ventilation but low or no perfusion.
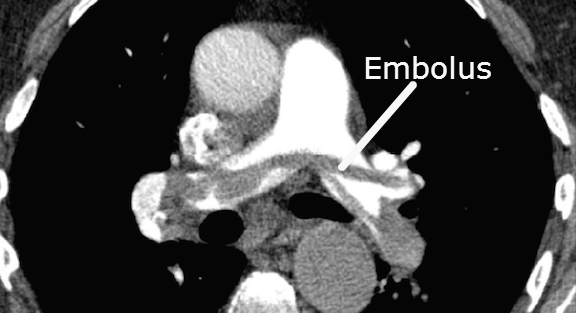
- Computed tomography (CT) Pulmonary angiography is perhaps the commonest test these days and involves giving IV contrast during Chest CT. The whole scan can be done in a single breath-hold. It is useful for identifying pulmonary emboli and can also identify other pathology. It is the best test in an unstable patient for a rapid diagnosis to facilitate urgent treatment.
- Pulmonary angiography is the gold standard but rarely done nowadays
CTPA anatomy
CTPA Example of PE
Differential
- Septic emboli from right sided valve e.g. tricuspid endocarditis in IV drug user
- Fat embolism (post-fracture)
- Air embolism (procedure related venous lines, diving).
- Post partum Amniotic fluid.
- Cancer and Neoplastic cells.
- Foreign materials may be procedure related
Management
- High FiO₂ (15L/min) oxygen, Cardiac monitoring BP, Pulse, O₂ saturation
- Suspected PE with haemodynamic instability: In suspected high-risk PE, as indicated by the presence of haemodynamic instability
- Bedside echocardiography or emergency CTPA (depending on availability and clinical circumstances) is recommended for diagnosis.
- It is recommended that IV anticoagulation with UFH, including a weight-adjusted bolus injection, be initiated without delay in patients with suspected high-risk PE.
Suspected PE stable patient
- Clinical assess: If PE suspected then calculate PE Wells score
- If Score <= 4: Check Dimer. If negative seek alternative cause and if positive then do CTPA and admit and treat
- If > 4 or more: Perform CTPA and if positive treat
- Initiation of anticoagulation is recommended without delay in patients with a high or intermediate clinical probability of PE while a diagnostic workup is in progress
- Analgesia - Opiates may be required
- Compromised SBP < 90 mmHg or other evidence to suggest massive PE
- Thrombolysis e.g. Alteplase should be considered in a patient with a large compromising PE where there is hypotension or signs of RV dysfunction. Possible strategy is Alteplase 10 mg IV over 1-2 minutes followed by 90 mg over 2 hours. A lower dose is given for those under the 65 Kg. There are various strategies. In dire circumstances doses given rapidly.
- Surgery such as open embolectomy to remove clot
- Interventional radiology to give thrombolysis directly or to agitate clot.
Suspected PE and Cardiac Arrest
- Usually seen as PEA. Low ETCO₂ readings (< 1.7 kPa or 13 mmHg) while performing high-quality CPR may support a diagnosis of pulmonary embolism, although it is a non-specific sign. Consider emergency echo if you have a skilled operator as an additional diagnostic tool.
- Give Thrombolysis when PE is the suspected cause of cardiac arrest. Then continue CPR for 60-90 minutes before termination. Consider the use of a mechanical chest compression device if prolonged CPR is needed.
- Also consider surgical embolectomy or percutaneous mechanical thrombectomy for cardiac arrest when PE is the known cause of cardiac arrest. Consider ECPR as a rescue therapy for selected patients with cardiac arrest when conventional CPR is failing in settings in which it can be implemented.
Anticoagulation and filters
- Enoxaparin (US Lovenox) 1.5 mg/kg per day ( a reduced dose given with renal impairment) as soon as there is clinical suspicion and stopped when PE has been disproved. If a PE is identified then Enoxaparin is continued until INR > 2.0
- Warfarin 3-6 months for a first Idiopathic PE is routine. Possibly shorter where there is an identifiable temporary precipitant. There should be an overlap of Warfarin and Heparin for the first 5 days with UFH or LMWH or Fondaparinux as there can exist a transient procoagulant condition until fully Warfarinised.
- IVC filters may be used where there is a high risk of VTE and anticoagulation is not possible in the short term or when PEs still recur despite anticoagulation. Patients should eventually be started on Warfarin. Newer devices can be removed after 6 weeks. The filters tend to clot off and can cause long term problems.
- Recurrent PE's get lifelong Warfarin or equivalent DOAC especially if no identifiable one event cause
Cancer
Edoxaban or Apixaban or rivaroxaban should be considered as an alternative to LMWH, with a word of caution for patients with gastrointestinal cancer due to the increased bleeding risk with NOACs.
Pregnancy
- A chest x-ray is not contraindicated in pregnancy. Any pregnant female presenting with shortness of breath should be reviewed by a senior member of the obstetric team, advice which comes from the RCOG.
- Enoxaparin dose should be doubled in pregnancy, due to the increased glomerular filtration rate (GFR) in pregnancy.
- D-dimers are always elevated in pregnancy, and are not helpful as a diagnostic aid, unless of course, they are low (very unlikely), thereby making the clinical suspicion of pulmonary embolism (PE) low.
- If DVT suspected then a doppler should be performed and if positive treat which also covers PE and means that with convincing clinical signs that PE may be inferred.
- For PE a CXR and Ventilation part of scanning may be used. If the diagnosis is still unclear a CTPA may be needed especially where there has been preceding lung disease.
- Warfarin is teratogenic in pregnancy and LMWH is usually given. Nearer delivery IV Heparin can be given and stopped prior to delivery and restarted afterwards.
- Misdiagnosis and failure to treat are more worrying than the exposure of the mother to radiation. The exposure of the fetus to radiation can usually be minimised.
- The main concern of CTPA is radiation exposure to the maternal breasts and long-term breast cancer risk. Take local advice as protocols vary.