Makindo Medical Notes.com |
|
|---|---|
| Download all this content in the Apps now Android App and Apple iPhone/Pad App | |
| MEDICAL DISCLAIMER:The contents are under continuing development and improvements and despite all efforts may contain errors of omission or fact. This is not to be used for the assessment, diagnosis or management of patients. It should not be regarded as medical advice by healthcare workers or laypeople. It is for educational purposes only. Please adhere to your local protocols. Use the BNF for drug information. If you are unwell please seek urgent healthcare advice. If you do not accept this then please do not use the website. Makindo Ltd | |
Anthrax (Bacillus anthracis)
-
| About | Anaesthetics and Critical Care | Anatomy | Biochemistry | Cardiology | Clinical Cases | CompSci | Crib | Dermatology | Differentials | Drugs | ENT | Electrocardiogram | Embryology | Emergency Medicine | Endocrinology | Ethics | Foundation Doctors | Gastroenterology | General Information | General Practice | Genetics | Geriatric Medicine | Guidelines | Haematology | Hepatology | Immunology | Infectious Diseases | Infographic | Investigations | Lists | Microbiology | Miscellaneous | Nephrology | Neuroanatomy | Neurology | Nutrition | OSCE | Obstetrics Gynaecology | Oncology | Ophthalmology | Oral Medicine and Dentistry | Paediatrics | Palliative | Pathology | Pharmacology | Physiology | Procedures | Psychiatry | Radiology | Respiratory | Resuscitation | Rheumatology | Statistics and Research | Stroke | Surgery | Toxicology | Trauma and Orthopaedics | Twitter | Urology
Early diagnosis of anthrax and initiation of appropriate treatment, particularly administration of a combination of antimicrobial drugs, are critical to improving survival
About
- Anthrax is the Greek word for coal, in reference to the black skin lesions victims develop in a cutaneous skin infection.
- Anthrax is due to bacillus anthracis and is a zoonotic infection usually acquired from herbivores and their hides.
Characteristics
- It is gram +ve and aerobic and forms spores
- Capsulated which consists of a polypeptide or D-Glutamic acid when in vivo
Source
- Found in soil from infected carcasses, wools, hides, bones
- It is most commonly an infection of animals but can be passed to man
- Animals are vaccinated in the US where thye have had previous anthrax
- Areas where found endemically
- Central/South America
- Sub-Saharan Africa,
- Asia, South/Eastern Europe
- Caribbean.
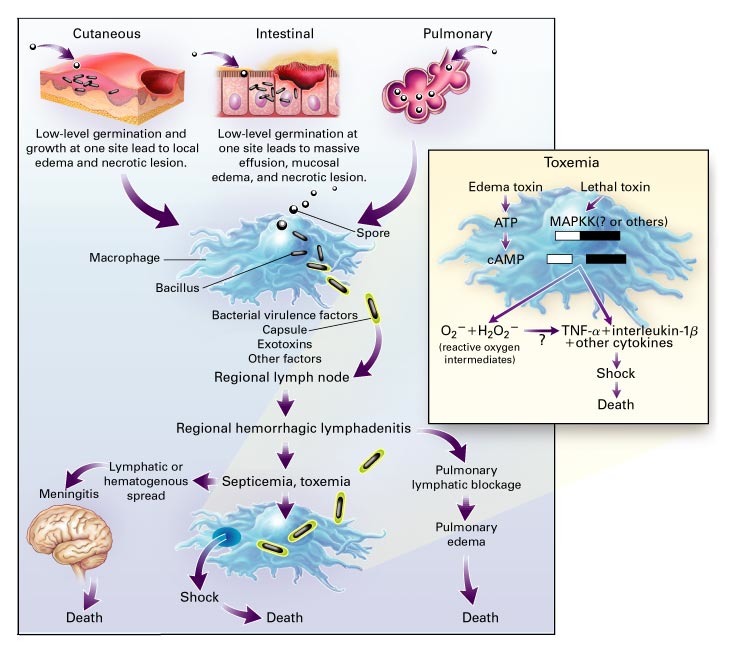
Virulence - Toxin production and capsule
- Protective antigen, a protein that binds to cells and forms channels and allows LF and EF to enter cells
- Lethal factor (LF) - a protease of Mitogen-activated protein kinase (MAP kinase)
- Oedema factor (EF) a calmodulin activated adenylate cyclase
- These factors tend to produce marked oedema and haemorrhage
- Antiphagocytic capsule
Pathophysiology
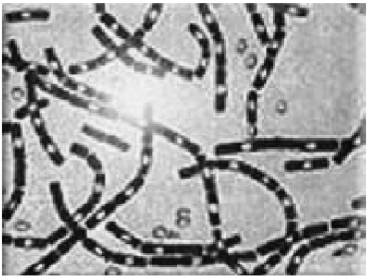
Microscopy
Clinical Pathogenicity
- Cutaneous
- Infection via skin abrasions from Hides and bones to form a black eschar with a localised haemorrhagic lymphadenitis
- Often seen with people handling hides in dock workers where spores got through abraded skin to cause a local and then systemic response
- Inhalational (Mortality> 50%)
- 'Wool sorters disease' with SOB, fever, shock, chest pain
- Also could be form of bioterrorism
- Progressive cyanosis, hypoxia, effusions and widened mediastinum on CXR
- Develops a haemorrhagic mediastinitis and shock
- Gastrointestinal
- Due to ingestion of meat products
- Nausea, Vomiting, Abdominal pain and bloody diarrhoea
- May cause progressive symptoms and even death
- Shock/Sepsis
- Hypotension, renal failure, Microangiopathic haemolytic anaemia
- Coagulopathy, thrombocytopenia, and haemorrhage
- Meningitis and haemorrhagic brain parenchymal infection
Investigations
- Isolation of the organism - Spores seen with modified Ziehl Nielsen stain
- McFadyen's reaction demonstrates bacilli in blood by heat fixing with polychrome methylene blue showing blue bacilli and surrounding pink capsular debris
- Serology for capsular antigen
- CXR: mediastinal widening
- CT chest: mediastinal involvement
Among patients with inhalation anthrax antimicrobial drug combination therapy was more likely to be curative than antimicrobial drug monotherapy
CXR showing mediastinal widening
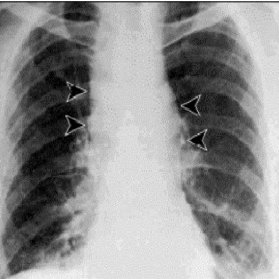
CXR several hours before death

Management: Discuss with Infectious Diseases early
References