Makindo Medical Notes.com |
|
|---|---|
| Download all this content in the Apps now Android App and Apple iPhone/Pad App | |
| MEDICAL DISCLAIMER:The contents are under continuing development and improvements and despite all efforts may contain errors of omission or fact. This is not to be used for the assessment, diagnosis or management of patients. It should not be regarded as medical advice by healthcare workers or laypeople. It is for educational purposes only. Please adhere to your local protocols. Use the BNF for drug information. If you are unwell please seek urgent healthcare advice. If you do not accept this then please do not use the website. Makindo Ltd | |
Ventricular Tachycardia (VT)
-
| About | Anaesthetics and Critical Care | Anatomy | Biochemistry | Cardiology | Clinical Cases | CompSci | Crib | Dermatology | Differentials | Drugs | ENT | Electrocardiogram | Embryology | Emergency Medicine | Endocrinology | Ethics | Foundation Doctors | Gastroenterology | General Information | General Practice | Genetics | Geriatric Medicine | Guidelines | Haematology | Hepatology | Immunology | Infectious Diseases | Infographic | Investigations | Lists | Microbiology | Miscellaneous | Nephrology | Neuroanatomy | Neurology | Nutrition | OSCE | Obstetrics Gynaecology | Oncology | Ophthalmology | Oral Medicine and Dentistry | Paediatrics | Palliative | Pathology | Pharmacology | Physiology | Procedures | Psychiatry | Radiology | Respiratory | Resuscitation | Rheumatology | Statistics and Research | Stroke | Surgery | Toxicology | Trauma and Orthopaedics | Twitter | Urology
Related Subjects: |Ventricular Fibrillation |Classical Ventricular Tachycardia |Idiopathic Ventricular Tachycardia |Resuscitation - Adult Tachycardia Algorithm |Resuscitation - Advanced Life Support |Automatic Implantable Cardioverter Defibrillator (AICD) |Brugada Syndrome |Long QT syndrome (LQTS) Acquired |Long QT syndrome (LQTS) Congenital |Torsades de Pointes |Wolff-Parkinson White syndrome (WPW) |Supraventricular Tachycardia (SVT) |Atrial Flutter |Atrial Fibrillation
Ensure that you have a defibrillator close by and switched on and you know how to use it. Follow Adult tachycardia algorithm as linked above.
| Management Summary: IV Access and get Defibrillator |
|---|
|
About
- More than 3 beats regular broad complex tachycardia rate > 120/min.
- Commonest cause is Ischaemic Heart Disease.
- Some patients may appear stable but can quickly decompensate so all must be treated as having the potential to cardiac arrest.
- Admit CCU. Instant access to defibrillation is vital in all cases
Types
- Sustained VT: lasts more than 30 seconds
- Non-Sustained VT: It is defined as 3 (sometimes 5) or more consecutive beats arising below the AVN with an RR interval of <600 ms (>100 beats/min) and lasting <30s
Causes
- Ischaemic cardiomyopathy
- LVH e.g. Hypertension
- Idiopathic dilated cardiomyopathy
- Brugada syndrome
- Arrhythmogenic right ventricular cardiomyopathy
- Myocarditis
- Cardiomyopathy e.g. HCM, DCM
- Overdose: Tricyclic overdose, Digoxin, antiarrhythmics
- Hypo/hyperkalaemia, Hypomagnesaemia
- Cocaine, Phaeochromocytoma
- Cong/Acquired Long QT syndromes
- RVOT Ventricular tachycardia with LBBB and RAD
Clinical
- Broad spectrum from mild symptoms and palpitation to cardiac arrest.
- Pulmonary oedema, Hypotension, Syncope, Presyncope
- Chest pain, Dizziness,
- Cannon a" wave in JVP, Depends on rate and LV function
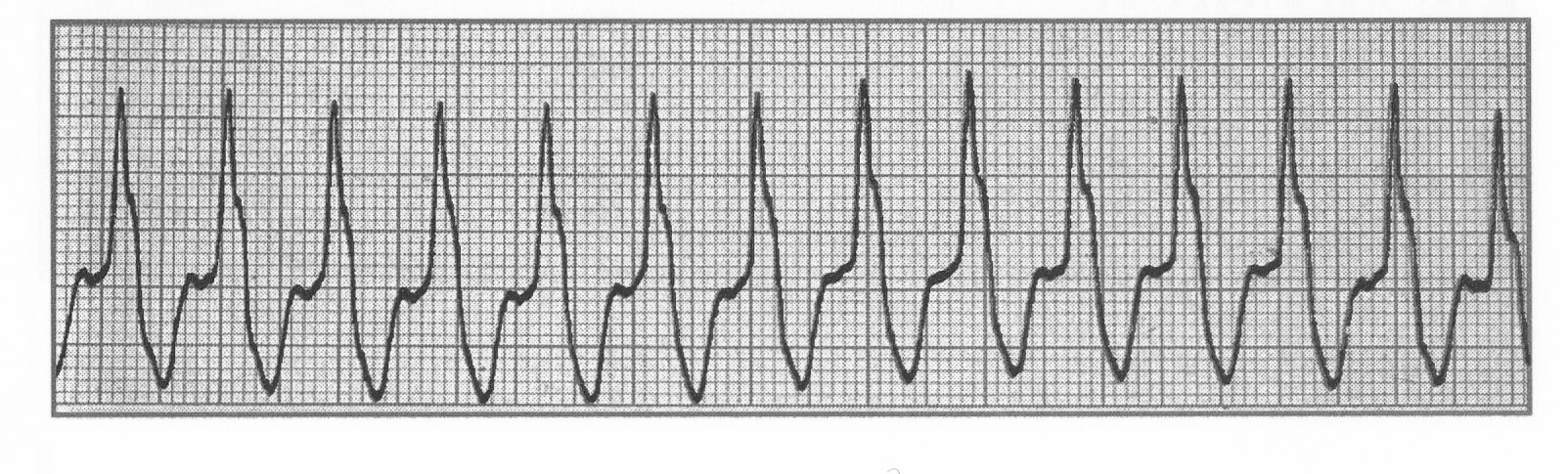
Rhythm Strips ECG Ventricular Tachycardia
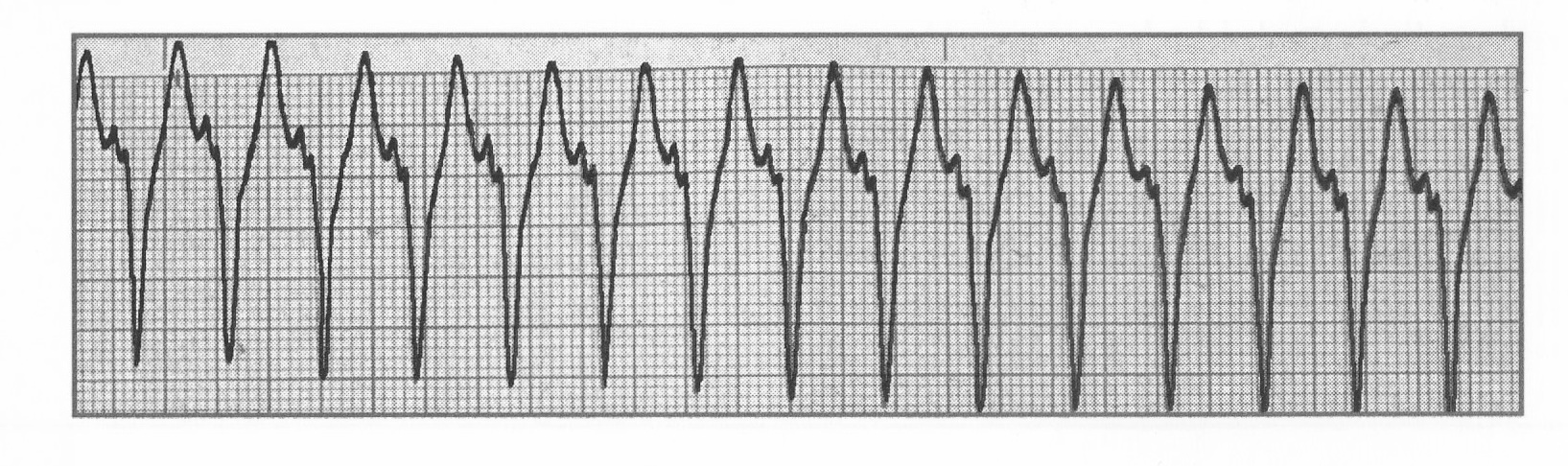
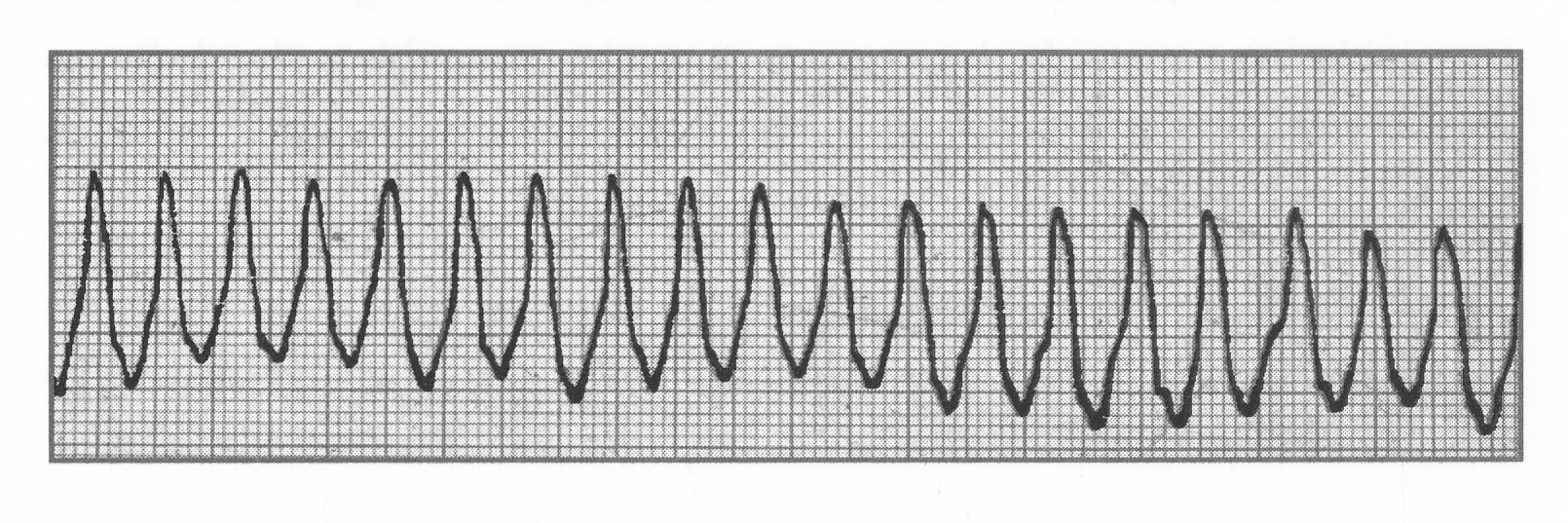
12 lead Ventricular Tachycardia

VT more likely if
- Fusion beats, Capture (narrow) beats, IHD, structural heart disease
- No RS wave on chest leads, AV dissociation
- RBBB > 0.14 secs LBBB > 0.16 secs, Extreme LAD, Extreme R to R regularity
Differential Regular wide rhythm >120/min
- Ventricular tachycardia,
- Atrial flutter with BBB (150/min)
- SVT with BBB (BBB: bundle branch block)
- Severe hyperkalaemia
- Pre-excited Atrial tachycardia
Investigations
- Check FBC, U&E, Mg, Ca, Lactate, ABG if needed.
- Urgent ECG: wide QRS > 3 small squares, regular.
- Troponin, BNP levels, Echocardiogram.
- Coronary Angiography and PCI if chest pain and ? STEMI
Classical VT is by far the most common cause of wide complex regular tachycardia, and there is no perfectly reliable way to distinguish classic VT with all its dangers from idiopathic VT or SVT with aberrancy on the surface 12-lead ECG. Treat as Classical VT - follow Adult tachycardia algorithm above
Acute Management
- ABC. If pulseless then CPR +DC shock. O₂ as per guidelines. IV 500 mls with 20 mmol KCl to keep potassium > 4.5 mmol/l + oral supplements. Revascularisation if STEMI or severe ischaemic basis suspected
- Stable: urgent 12 lead ECG, IV access. Bloods. Monitor. Be ready to give a DC shock.
- Pharmacological choices if stable
- IV Metoprolol 5 mg
- IV Amiodarone 300 mg over 30 mins and then 900 mg over 24hrs through central line.
- IV Lidocaine 50 mg over 2 minutes. Can be repeated every 5 minutes to a max 200 mg
- IV Magnesium Sulphate 2 g (8 mmol) over 15 mins
- Unstable/ Pulseless: ABC, DC countershock. Bloods. Consider IV Amiodarone.
- ACS/STEMI then treat/PCI. Look for and treat cause. Correct electrolytes.
- Long term
- Non sustained VT: Consider Beta blockers. Where LV function (EF<30%) is poor consider for AICD
- Long term: Chronic prophylactic antiarrhythmic drug therapy. Investigating cause Echo, possibly Angiography and Electrophysiological studies, Holter monitoring.
- AICD: Those who survive the first episode of life-threatening ventricular arrhythmia are at high risk of further episodes and an ICD should be considered.
- Catheter Ablation may be considered