Makindo Medical Notes.com |
|
|---|---|
| Download all this content in the Apps now Android App and Apple iPhone/Pad App | |
| MEDICAL DISCLAIMER:The contents are under continuing development and improvements and despite all efforts may contain errors of omission or fact. This is not to be used for the assessment, diagnosis or management of patients. It should not be regarded as medical advice by healthcare workers or laypeople. It is for educational purposes only. Please adhere to your local protocols. Use the BNF for drug information. If you are unwell please seek urgent healthcare advice. If you do not accept this then please do not use the website. Makindo Ltd | |
Acute Anaphylaxis
-
| About | Anaesthetics and Critical Care | Anatomy | Biochemistry | Cardiology | Clinical Cases | CompSci | Crib | Dermatology | Differentials | Drugs | ENT | Electrocardiogram | Embryology | Emergency Medicine | Endocrinology | Ethics | Foundation Doctors | Gastroenterology | General Information | General Practice | Genetics | Geriatric Medicine | Guidelines | Haematology | Hepatology | Immunology | Infectious Diseases | Infographic | Investigations | Lists | Microbiology | Miscellaneous | Nephrology | Neuroanatomy | Neurology | Nutrition | OSCE | Obstetrics Gynaecology | Oncology | Ophthalmology | Oral Medicine and Dentistry | Paediatrics | Palliative | Pathology | Pharmacology | Physiology | Procedures | Psychiatry | Radiology | Respiratory | Resuscitation | Rheumatology | Statistics and Research | Stroke | Surgery | Toxicology | Trauma and Orthopaedics | Twitter | Urology
Related Subjects: |Adrenaline/Epinephrine |Atropine |Adult Resus:Acute Anaphylaxis |Adult Resus:Basic Life Support |Adult Resus: Advanced Life Support |Adult Resus: Obstetric Cardiac Arrest |Newborn/Child Resus: All |Acute Hypotension |Cardiogenic shock |Distributive Shock |Hypovolaemic or Haemorrhagic Shock |Obstructive Shock |Septic Shock and Sepsis |Shock (General Assessment) |Toxic Shock Syndrome |Respiratory failure |Resus:Bradycardia |Resus:Tachycardia |Resus:Hyperkalaemia |Resus:Post Resuscitation Algorithm |Resus:Acute Severe Asthma |Resus:Acute Haemorrhage |
Anaphylaxis is a severe, life-threatening, generalised or systemic hypersensitivity reaction. Adrenaline 0.5 mg (0.5 ml) IM of 1:1000 is potentially life-saving and must therefore promptly be administered as the first-line treatment for the emergency management of anaphylaxis. It is given through clothes if needed IM into the lateral thigh
| Acute Anaphylaxis |
|---|
First steps
Initial Management Summary: Resuscitation UK
Refractory Anaphylaxis
|
Treat if there are any Life-threatening ABC features: Hoarse voice, stridor, increased work of breathing, wheeze, fatigue, cyanosis, SpO₂ <94%, Low blood pressure, signs of shock, confusion, reduced consciousness. Rash alone is not listed but be observant for ongoing changes.
Swelling of lips, tongue, pharynx, and epiglottis may lead to complete upper airway occlusion. Lower airway involvement is similar to acute severe asthma — dyspnoea, wheeze, chest tightness, hypoxia, and hypercapnia
Introduction
- Anaphylaxis is a potentially fatal reaction to an allergen.
- Adrenaline given IM improves prognosis and can be life-saving.
- Adrenaline IM should be given where there is clinical suspicion of anaphylaxis.
- The key signs are hypotension or skin changes or wheeze or stridor.
- Always summon senior help such as 999 immediately if no rapid recovery.
- In hospital call for the medical emergency team.
- Never give IV Adrenaline (Epinephrine) in anaphylaxis.
- IV Adrenaline should only be used in cardiac arrest protocol.
Aetiology
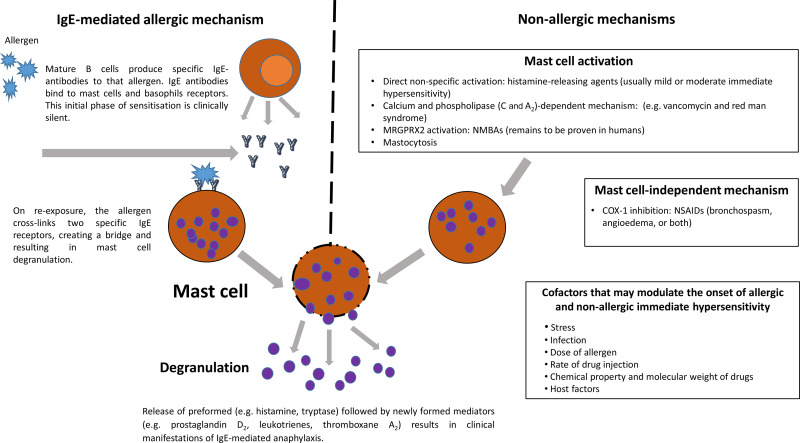
- With anaphylaxis there is Mast cell degranulation due to antigen cross linking IgE on cell surface.
- This leads to the systemic release of histamine which binds to H1, H2, H3 and H4 receptors.
- There is then a massive release of cytokines and chaemokines.
- Requires prior exposure and formation of allergen specific IgE.
- Increased post capillary venule permeability oedema.
- Vascular smooth muscle relaxation - hypotension
Causes
- Causative agents, Drugs e.g. Penicillin, Radiological contrast media.
- Insect stings, Eggs, Fish, Peanuts, Latex.
- Giving blood products e.g. IVIG to those with selective IgA deficiency
Clinical
- Feeling faint, breathless, wheezing, stridor, clammy skin, confusion and anxiety
- Collapsing or losing consciousness, Colic and diarrhoea and vomiting
- Abdominal pain, flushing, Wheeze, Urticaria (not with C1 esterase deficiency)
- Facial, lips swell, Laryngeal oedema can compromise airway - stridor
Differential
- Septic shock: warm, vasodilated. Blood cultures, FBC, CRP, lactate if sepsis considered. IV fluids.
- Scombroidosis (Histamine)
- Systemic mastocytosis
- Faint (vasovagal episode).
- Panic attack.
- Breath-holding episode in child.
- Idiopathic (non-allergic) urticaria or angioedema.
- Phaeochromocytoma
- Hereditary angioedema.
Investigation
- FBC, U&E, LFTs, Lactate, ABG may be needed
- Mast cell tryptase (level reflects the degree of hypotension) should be sent within 1 hour and 24 hours (or at follow up). It may not be elevated in food allergy. Send 10 mL of clotted blood should be taken within 60 min of the reaction for confirmation of the diagnosis: e.g. by measurement of the mast cell tryptase. Serum should be separated and stored at -20°C.
- Later at an Immunology clinic - Allergen skin testing, RAST - identifies specific IgE
Prevention
- Mistakes in cross matching or patient identification and giving the wrong blood
- Avoiding Penicillin or other drugs when allergic
- Avoiding food allergies
- Having access to an EpiPen
Management
- Assess ABCDE. Lay patient supine and raise legs/end of the bed if anaphylaxis possible. Call MET team. Get senior help quickly if fails to respond.
- Stop causative drug or infusion or blood product, remove bee sting.
- If airway issues get the anaesthetic team. HR, BP, Telemetry, sats
- Give O₂ High flow 15L/min target 94-98%. Non-rebreather mask. May have to give less if COPD
- Give Adrenaline (Epinephrine in US) 0.5 ml of 1 in 1000 stat IM. May be repeated at 5-minute intervals depending on the response. Give IM into the anterolateral aspect of the middle third of the thigh using a needle long enough to ensure the Adrenaline (Epinephrine) is given into the muscle. This can be given through clothes. Do not give IV Adrenaline unless cardiac arrest.
- IV 500-1000 mls stat 0.9% N-Saline and titrate to BP and clinical status. Some may need several litres. Watch for overload in an older patient
Deprecated Treatments now
- Salbutamol (Albuterol in US) 5mg and nebulise with O₂ if patient wheezy
- Hydrocortisone 200 mg stat and 8-hourly as needed IV/IM and may be used as they may reduce the risk of late-phase respiratory symptoms
- Antihistamine Chlorphenamine 10 mg stat IV (UK) or Benadryl/Diphenhydramine 25-50 mg stat IV(USA) and Ranitidine may also be given. Systemic H1-(& H2)-antihistamines may relieve cutaneous symptoms of anaphylaxis
- Monitor for 6-12 hours following full recovery to ensure no late reactions. Such biphasic responses can occur. Before discharge, the risk of future reactions should be assessed and an adrenaline auto-injector should be prescribed to those at risk of recurrence. Ensure if given Epipens also instructed how to use it. Arrange or advise referral to a specialist for allergy clinic or immunology opinion and identification of cause and antigen avoidance.