Makindo Medical Notes.com |
|
|---|---|
| Download all this content in the Apps now Android App and Apple iPhone/Pad App | |
| MEDICAL DISCLAIMER:The contents are under continuing development and improvements and despite all efforts may contain errors of omission or fact. This is not to be used for the assessment, diagnosis or management of patients. It should not be regarded as medical advice by healthcare workers or laypeople. It is for educational purposes only. Please adhere to your local protocols. Use the BNF for drug information. If you are unwell please seek urgent healthcare advice. If you do not accept this then please do not use the website. Makindo Ltd | |
Moyamoya disease
-
| About | Anaesthetics and Critical Care | Anatomy | Biochemistry | Cardiology | Clinical Cases | CompSci | Crib | Dermatology | Differentials | Drugs | ENT | Electrocardiogram | Embryology | Emergency Medicine | Endocrinology | Ethics | Foundation Doctors | Gastroenterology | General Information | General Practice | Genetics | Geriatric Medicine | Guidelines | Haematology | Hepatology | Immunology | Infectious Diseases | Infographic | Investigations | Lists | Microbiology | Miscellaneous | Nephrology | Neuroanatomy | Neurology | Nutrition | OSCE | Obstetrics Gynaecology | Oncology | Ophthalmology | Oral Medicine and Dentistry | Paediatrics | Palliative | Pathology | Pharmacology | Physiology | Procedures | Psychiatry | Radiology | Respiratory | Resuscitation | Rheumatology | Statistics and Research | Stroke | Surgery | Toxicology | Trauma and Orthopaedics | Twitter | Urology
Related Subjects:
|Subarachnoid Haemorrhage
|Haemorrhagic stroke
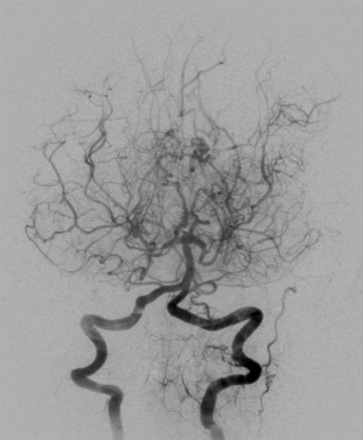
This is a non-inflammatory vasocclusive disease of ICA, MCA and ACA and is a cause of both ischaemic and to a lesser extent haemorrhagic stroke. The abnormal net-like vessels at the base of the brain seen in cerebral angiograms of this disease were described by most native speakers of Japanese as "Moyamoya," a Japanese expression for something hazy, such as a puff of cigarette smoke drifting in the air. The name was popularised by Jiro Suzuki. [Suzuki J et al. 1983]
About
Genetics
Aetiology
Associations
Clinical
Investigations
Stage Description
1 Stenosis of the suprasellar ICA usually bilateral
2 Development of Moyamoya vessels with dilatation of all main cerebral arteries at base of brain
3 Increasing ICA stenosis and prominence of Moyamoya vessels with reduction of flow in the middle and anterior cerebral arteries
4 Entire Circle of Willis and PCAs occluded. Extracranial collateralisation with minimisation of Moyamoya vessels. Proximal portions of the posterior cerebral arteries become involved
5 Reduction of Moyamoya and absence of all main cerebral arteries
6 Disappearance of Moyamoya vessels and major cerebral vessels; the cerebral circulation is supplied only by the external carotid system
Management
Further Reading