Makindo Medical Notes.com |
|
|---|---|
| Download all this content in the Apps now Android App and Apple iPhone/Pad App | |
| MEDICAL DISCLAIMER:The contents are under continuing development and improvements and despite all efforts may contain errors of omission or fact. This is not to be used for the assessment, diagnosis or management of patients. It should not be regarded as medical advice by healthcare workers or laypeople. It is for educational purposes only. Please adhere to your local protocols. Use the BNF for drug information. If you are unwell please seek urgent healthcare advice. If you do not accept this then please do not use the website. Makindo Ltd | |
Acute Coronary Syndrome (ACS) NSTEMI USA
-
| About | Anaesthetics and Critical Care | Anatomy | Biochemistry | Cardiology | Clinical Cases | CompSci | Crib | Dermatology | Differentials | Drugs | ENT | Electrocardiogram | Embryology | Emergency Medicine | Endocrinology | Ethics | Foundation Doctors | Gastroenterology | General Information | General Practice | Genetics | Geriatric Medicine | Guidelines | Haematology | Hepatology | Immunology | Infectious Diseases | Infographic | Investigations | Lists | Microbiology | Miscellaneous | Nephrology | Neuroanatomy | Neurology | Nutrition | OSCE | Obstetrics Gynaecology | Oncology | Ophthalmology | Oral Medicine and Dentistry | Paediatrics | Palliative | Pathology | Pharmacology | Physiology | Procedures | Psychiatry | Radiology | Respiratory | Resuscitation | Rheumatology | Statistics and Research | Stroke | Surgery | Toxicology | Trauma and Orthopaedics | Twitter | Urology
Related Subjects: |Atherosclerosis |Ischaemic heart disease |Assessing Chest Pain |Acute Coronary Syndrome (ACS): Complications |ACS - General |ACS - STEMI |ACS - NSTEMI |ACS - GRACE Score |ACS - ECG Changes |ACS -Cardiac Troponins |ACS - Post MI arrhythmias |ACS: Right Ventricular STEMI |ACS: Sgarbossa Criteria
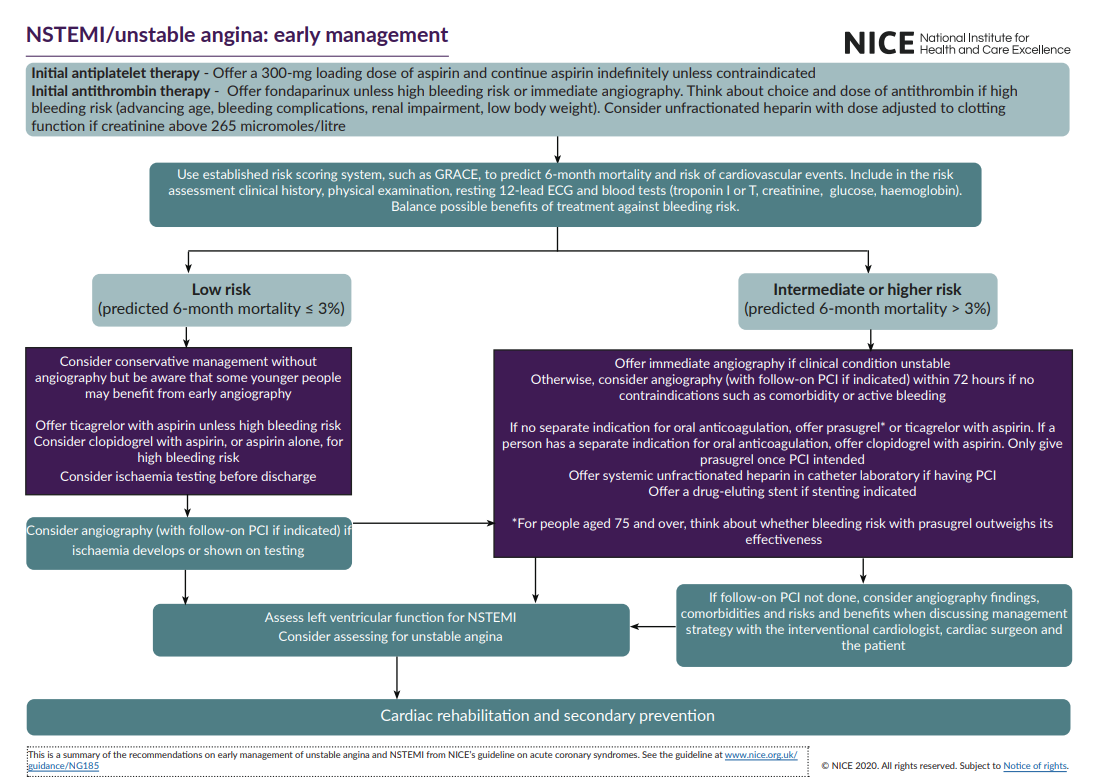
All ACS including STEMI and NSTEMI can present atypically, especially in women, older adults, and people with diabetes. Risk assessment in patients with Non-ST-Elevation Myocardial Infarction (NSTEMI) is crucial for guiding treatment decisions and predicting outcomes. A more interventional approach - i.e. PCI may be suited for higher risk patients - these are older, diabetes, heart failure, CKD, hypotensive, tachycardic, prolonged or recurrent chest pain, high troponin and ST depression or T wave inversion and a prior history of MI or PCI/CABG. There are various scores such as GRACE and TIMI and HEART.
| Management of ACS/NSTEMI: Repeat ECG every 15-20 mins |
|---|
|
Acute Management of Non-ST Acute Coronary Syndrome: Standard + Angiography for high-risk patients
Introduction
- Presents typically as chest pain +/- ECG changes. If the Cardiac Troponin meets the definition of an MI then NSTEMI is diagnosed else the diagnosis is Unstable angina or another cause of chest pain.
- It is important to realise that other things cause chest pain and troponin rises e.g. PE, Myocarditis, Takotsubo.
- If the patient is felt to be at high risk for further events then angiography may be considered.
Aetiology
- Usually due to a Partially Occluded coronary artery
- There may be myocardial necrosis and raised troponin
Classification
- If troponin elevated = myocardial damage then NSTEMI
- If troponin not elevated then Unstable angina
Suspect diagnosis if
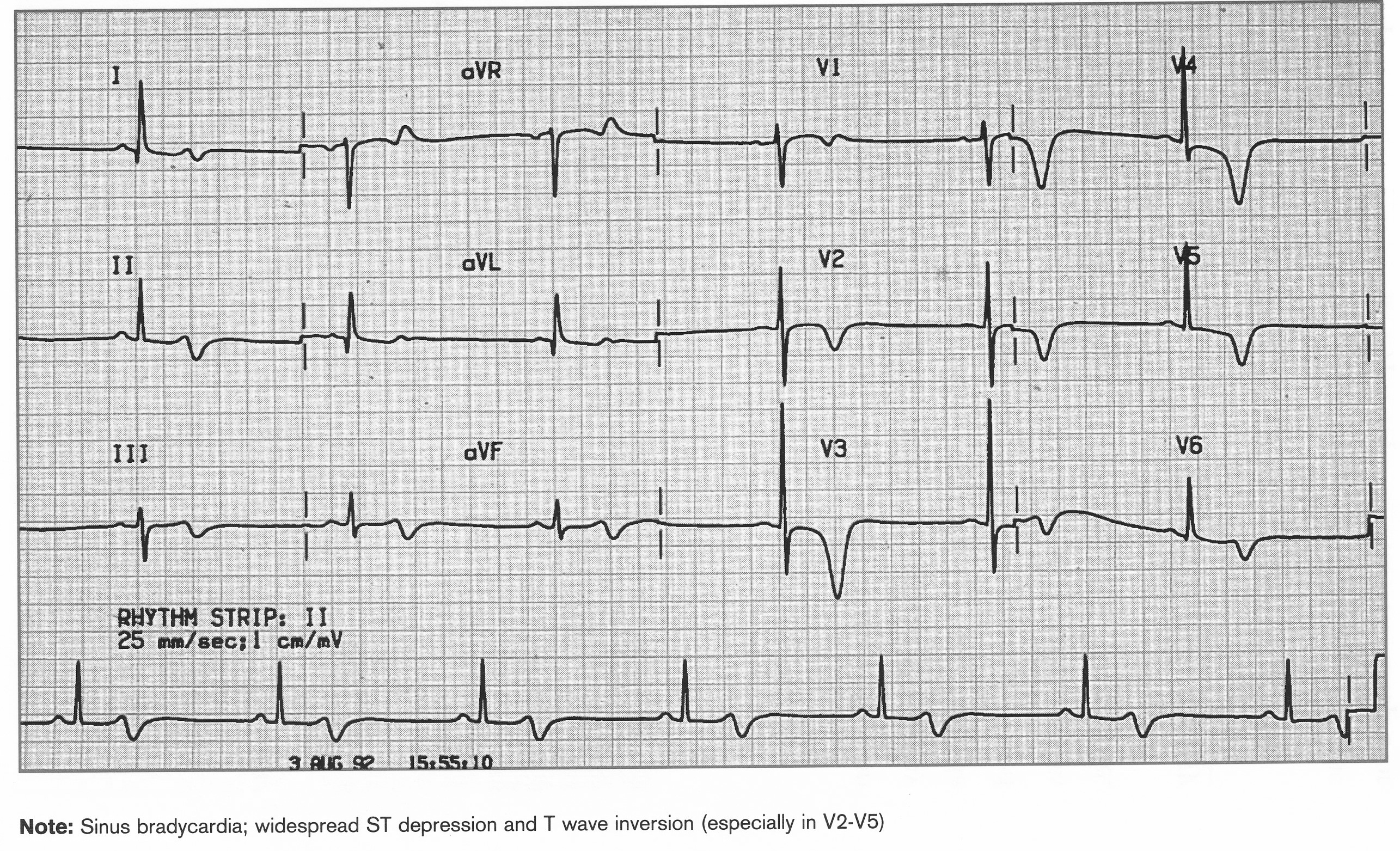
- Ischaemic sounding chest pain + ECG changes (new / deeper T wave inversion, new ST depression
- If the GRACE 2 score is > 140, or there are other features of High-Risk ACS (persistent ST depression > 1mm and on-going chest pain, T wave inversion or biphasic T waves in leads V1-V4 Wellen's syndrome) you should contact cardiology immediately
Medications
- Give Oxygen to achieve SaO2 94-98%
- GTN 400 mcg per spray or S/L GTN tablet (300 or 500 mcg) if Chest pain, SBP > 110 mmHg, LVF
- Pain relief: Morphine 5-10 mg IV or Diamorphine 2.5-5 mg IV
- Antiemetic: Metoclopramide 10 mg IV Oxygen and Monitor
- Antiplatelet: Aspirin 300 mg PO stat
- Commence a P2Y12 antagonist: one of the following (discuss with cardiology if risk of bleeding)
- Clopidogrel 300-600 mg PO Stat
- Ticagrelor 180 mg PO stat
- Prasugrel 60 mg PO stat
- Metoprolol 5-15 mg IV or 50 mg PO BD if LV dysfunction, Tachycardia (not if Asthma or Pulmonary oedema). Alternatives are Diltiazem for those who cannot take a beta blocker.
- Furosemide 40-80 mg IV if pulmonary oedema
- Fondaparinux 2.5 mg OD SC may be given if no reperfusion therapy
- Hyperglycaemia
- Check blood glucose on admission, and check fasting blood glucose at day 4 or HBA1C predischarge for anyone with hyperglycaemia at presentation (blood glucose >11mMol/L).
- Glucose control is important (aim BM 6-11 mmol/L), but take care to avoid hypoglycaemia (BM <4.4) which can worsen outcomes in diabetic patients with acute coronary syndromes.
- If control poor in the CCU then consider starting VRII.
Risk Assess: choose one of these on specialist advice
- In those with NSTEACS (USA/NSTEMI) the focus on the selection of angiography and intervention and patients are selected on basis of risk scores which calculates the expected risk of mortality. These include TIMI and GRACE scores.
- TIMI Risk Score for USA/NSTEMI can be done by hand or using Online calculator
- Age = 65 years? Yes +1
- > 3 Risk Factors for CAD? Yes +1 (HTN,Smoker,Chol,DM,FHX)
- Known CAD (stenosis = 50%)? Yes +1
- Aspirin use in the past 7 days? Yes +1
- Severe angina (= 2 episodes < 24 hrs)? Yes +1
- ST changes = 0.5mm? Yes +1
- + Cardiac Marker? Yes +1
- Risk score 0-7.
- A score of 6-7 = 41% risk at 14 days of: all-cause mortality, new or recurrent MI, or severe recurrent ischaemia requiring urgent revascularization.
- Global Registry of Acute Coronary Events score (GRACE) see Online calculator here
- Age
- Heart rate
- Systolic BP
- Creatinine
- Killip class (heart failure)
- Cardiac arrest at admission
- Elevated biomarkers
- ST segment deviation
- Higher risk 6 month mortality > 3% then consider Angiography +/- PCI
- Higher risk if raised troponin, ST/T wave changes, diabetes, CKD, LVEF<40%, early angina, post PCI, prior CABG. May require Tirofiban infusion and angiography.
- Low risk normal troponin, normal ECG, no further angina no heart failure. Consider OP Exercise stress test.
Two-dimensional echocardiography in ACS
- Has become a useful bedside technique in the triage of patients with acute chest pain where the diagnosis might be in doubt with indeterminate ECG changes.
- Regional wall motion abnormalities occur almost instantaneously after coronary occlusion and well before necrosis. However, wall motion abnormalities are not always specific for STEMI and may be due to ischaemia or an old infarction.
Very high-risk cases who should have angiography within hours (<2 hours by ESC guidelines) are those with at least one of the following:.
- Haemodynamic instability or cardiogenic shock thought to be due to ischaemia
- Recurrent or ongoing cardiac type chest pain refractory to medical treatment
- Life-threatening arrhythmias or cardiac arrest
- Mechanical complications of MI
- Acute heart failure (due to ECG or symptomatic evidence of ischaemia)
- Recurrent dynamic ST-T wave changes, particularly with intermittent ST elevation
High risk cases who should have urgent angiography (<24 hours by ESC guidelines) are those with at least one of the following:
- GRACE Score > 140
- Isolated (i.e. no other high-risk features) Troponin T value > 250 with a significant change (delta) over 2 measurements and presentation compatible with MI
- Dynamic ST-depression or deep T-wave inversion (symptomatic or silent), especially precordial leads (Wellen's pattern)
- For all other NSTEMI, the current NICE recommendation is for angiography within 72 hours
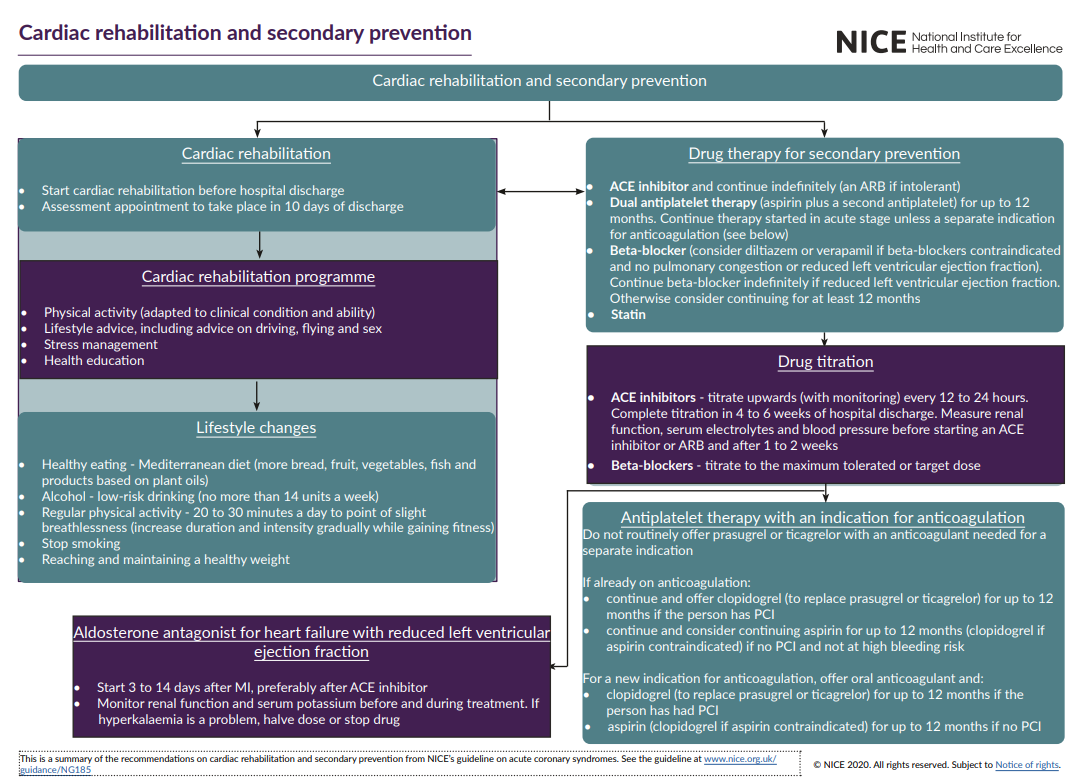
On Discharge
- Statin e.g. Atorvastatin 80mg po nocte. Statins have been shown to reduce mortality in patients with cardiovascular disease. More intensive lipid-lowering associated with reduced mortality in acute coronary syndromes
- ACEI. Once clinically and haemodynamically stable, start Ramipril at 2.5mg once or twice daily dependent on BP and renal function. Increase every 1-3 days in the hospital to a maximum of 5mg BD or 10 mg daily. Patients with LVSD EF<40% and/or NYHA class IV should be started on Ramipril 1.25mg daily and titrated gradually every 1-2 days to 10mg daily. Patients who don't tolerate ACEi because of cough should be switched to an angiotensin receptor blocker (e.g. Valsartan or losartan). Monitor renal function after initiation of ACEi or ARB
- Aldosterone antagonist ie. Eplerenone 25mg PO od Shown to improve outcome in patients with severe LV dysfunction post-STEMI in patients with LVEF<40% (with diabetes or signs of HF) post-MI. Monitor carefully for hyperkalaemia and monitor renal function after initiation
- Smoking cessation: Advice on the importance of smoking cessation. Nicotine replacement therapy should be offered and prescribed as required. Offer contact for community smoking cessation services if not ready at the moment to stop.
- Anticoagulation: provided there is no contraindication then the following patients should be anticoagulated: Consider prophylactic LMWH in patients with prolonged immobility post-MI (>24hrs). Continue Warfarin in all patients with a long-term indication for anticoagulation already on Warfarin therapy (e.g. mechanical valve, recurrent DVT/PE, chronic AF with high CHADSVaSc risk score) alongside antiplatelet therapy. Consider long term formal anticoagulation with Warfarin or a novel oral anticoagulant in patients with newly diagnosed atrial fibrillation guided by CHADS2 or CHADSVASc risk score (see AF guideline for further details) Anticoagulation with LMWH then Warfarin is indicated before discharge for patients with LV thrombus identified on echocardiography or a thromboembolic event post-MI
- Dietary advice: Encourage the consumption of a Mediterranean diet which should include oily fish or nuts if vegetarian, five portions of fruit and vegetables, reduced saturated fats and increase soluble fibre in the diet
- Exercise advice: On an individual basis, encourage early mobilisation and build up to the increased activity of 150 minutes per week of moderate-intensity.
- Home after several days if uncomplicated. Dietary advice. Cardiac rehab
- Smoking cessation. No added salt. Manage any diabetes and obesity