Makindo Medical Notes.com |
|
|---|---|
| Download all this content in the Apps now Android App and Apple iPhone/Pad App | |
| MEDICAL DISCLAIMER:The contents are under continuing development and improvements and despite all efforts may contain errors of omission or fact. This is not to be used for the assessment, diagnosis or management of patients. It should not be regarded as medical advice by healthcare workers or laypeople. It is for educational purposes only. Please adhere to your local protocols. Use the BNF for drug information. If you are unwell please seek urgent healthcare advice. If you do not accept this then please do not use the website. Makindo Ltd | |
Cauda Equina Syndrome
-
| About | Anaesthetics and Critical Care | Anatomy | Biochemistry | Cardiology | Clinical Cases | CompSci | Crib | Dermatology | Differentials | Drugs | ENT | Electrocardiogram | Embryology | Emergency Medicine | Endocrinology | Ethics | Foundation Doctors | Gastroenterology | General Information | General Practice | Genetics | Geriatric Medicine | Guidelines | Haematology | Hepatology | Immunology | Infectious Diseases | Infographic | Investigations | Lists | Microbiology | Miscellaneous | Nephrology | Neuroanatomy | Neurology | Nutrition | OSCE | Obstetrics Gynaecology | Oncology | Ophthalmology | Oral Medicine and Dentistry | Paediatrics | Palliative | Pathology | Pharmacology | Physiology | Procedures | Psychiatry | Radiology | Respiratory | Resuscitation | Rheumatology | Statistics and Research | Stroke | Surgery | Toxicology | Trauma and Orthopaedics | Twitter | Urology
Related Subjects: |Initial Trauma Assessment and Management |Thoracic Trauma Assessment and Management |Flail Chest Rib fractures |Resuscitative Thoracotomy |Haemorrhage control |Traumatic Brain Injury |Traumatic Cardiac Arrest |Abdominal trauma |Tranexamic Acid |Silver Trauma |Cauda Equina
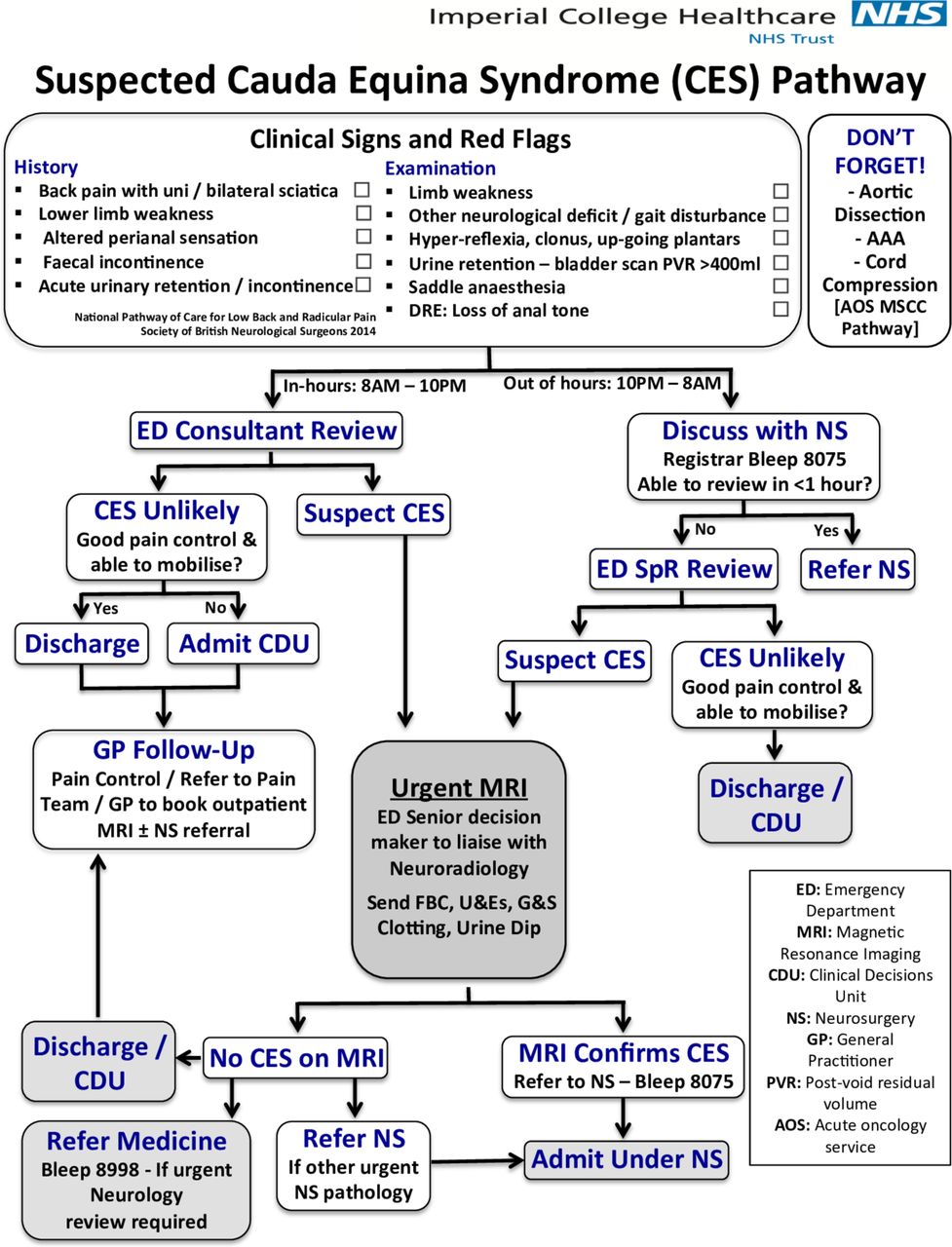
A patient presenting with acute low back pain with a suggestion of a disturbance of their bladder or bowel function and/or saddle sensory disturbance should be suspected of having CES
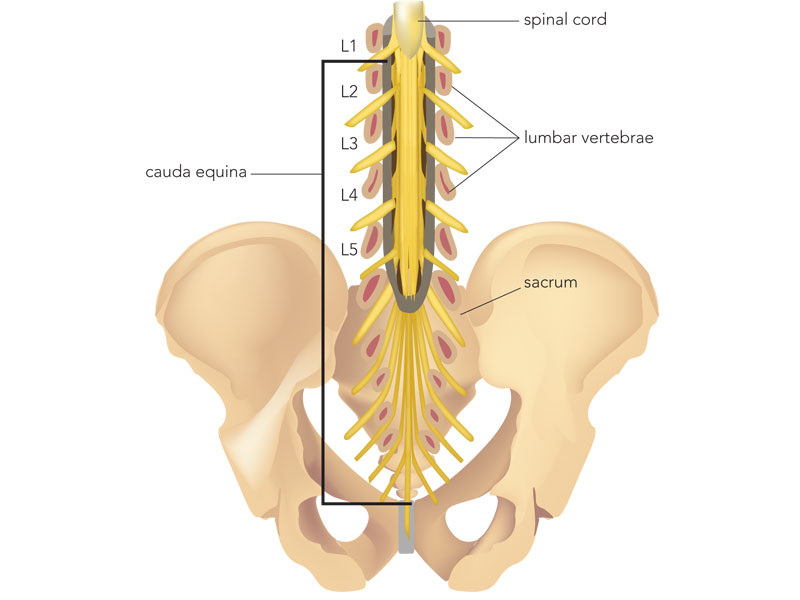
Anatomy
The cauda starts at L2 and contains LMN motor from lower lumbar and sacral roots and sphincters and afferent sensory from perianal and saddle areas. It lies below the cord which ends lower L1. There are no UMN signs unless the cord is also involved higher up which may suggest multiple lesions or If the lesion is at the filum terminale.
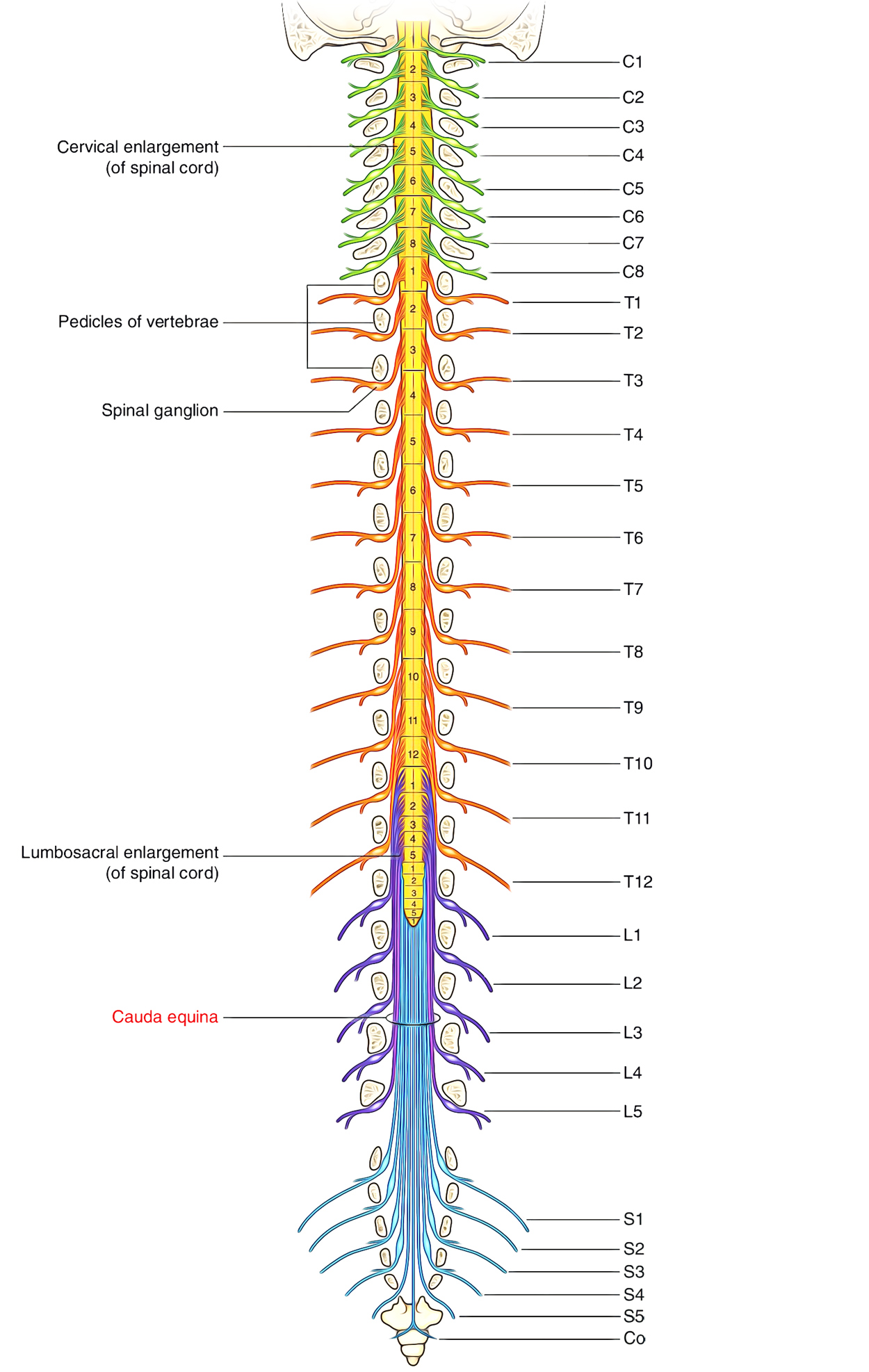
Anatomy with vertebrae
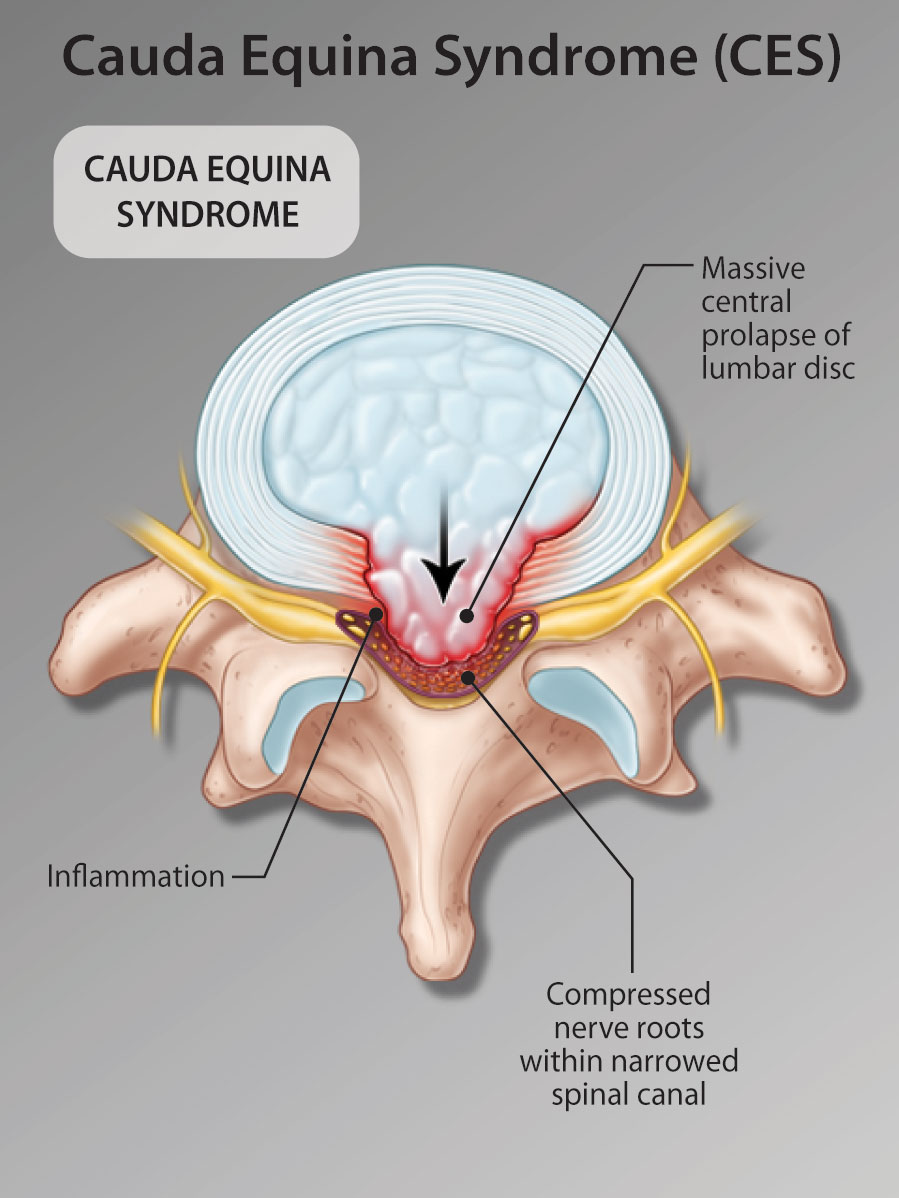
Anatomy with central disc compression of cauda
About
- Damage to nerve roots below L1/L2 where cord ends
- Most commonly due to prolapsed lumbar disc
- There is compression of lumbar and sacral roots
- This is a compressive radiculopathy
Aetiology
- Degenerative spinal disease/spinal stenosis
- Spinal fractures
- Central Lumbar disc herniation L4/5 or L5/S1
- Spinal metastatic bone disease
- Malignancy e.g. ependymoma of filum terminale
- Lipoma with spina bifida
- AV malformation and bleeding
- Dural AV fistulas
- Mass caused by infection or hematoma
- Fragment of bone from a retro-pulsed vertebral insufficiency fracture
The commonest cause of difficulties in passing urine in patients with lumbar degenerative disorders is pain and not a cauda equina syndrome but that does not exclude a cauda equina syndrome
Clinical
- Suden bilateral sciatica and lower back pain
- Usually loss of bladder control with overflow incontinence
- Loss of anal sphincters with incontinence
- Flaccid LMN weakness below lesion involving legs
- Sensory loss over the perianal region and saddle area and genitals
- Reduced lax anal sphincter with low tone and Reduced ankle jerks
- No UMN signs - plantars down going, reflexes normal or reduced unless the cord is also involved which may suggest multiple lesions or a lesion at the conus medullaris which affects cord and cauda together.
- Loss of normal sexual function
Patients at high risk of CES
- Bilateral radicular pain and/or bilateral sensory disturbance
- Bilateral motor weakness and/or bilateral loss of reflexes.
- These patients do not have a CES but they are at high risk.
Investigations
- FBC, U&E, LFTs, ESR, Ca, CXR, PSA, Myeloma screen
- Malignancy suspected: Breast exam and mammogram, Exclude melanoma
- CT CAP and tumour markers if tumour suspected
- Plain films are not useful for the diagnosis
- USS Bladder: The ultrasound assessment of residual bladder volume post voiding is commonly used in the emergency department to help test for CES. Again, whilst this is widely used, the evidence to support its validity in assessment for CES is not well established
- Urgent MRI or CT depending on local availability and if no contraindications to MRI scanning. Optimal same-day scanning where possible. Follow local guidelines.
THe four stages of CES
- CESS Suspected:
- Bilateral radicular pain
- CESI: Incomplete
- Urinary difficulties of neurogenic origin
- Altered urinary sensation
- Loss of desire to void
- Poor urinary stream
- Need to strain to micturate
- CESR Retention
- Neurogenic retention of urine
- Painless urinary retention and overflow
- Incontinence where the bladder is no longer under executive control
- CESC Complete
- Objective loss of CE function
- Absent perineal sensation
- Patulous anus (spread open)
- Paralysed insensate bladder and bowel
Outcomes from Imaging
- Cauda equina compression confirmed leading to immediate referral to an appropriate surgical service as below
- Cauda equina compression excluded but a potential structural explanation of pain identified. This should precipitate appropriate advice about potential future cauda equina symptoms and may include referral via local spinal pathways during working hours.
- Non-compressive pathology may be identified (e.g. demyelination) which should precipitate referral to the appropriate service.
- No explanation of the patient’s symptoms may be apparent. An appropriate plan for further management is required and may include a cervicothoracic MRI and referral to continence services
Management
- Cauda equina syndrome (CES) is a devastating condition for quality of life that may lead to permanent loss of bladder, bowel and sexual function with associated neurological pain affecting the patient, their family and relationships. It is a time-sensitive syndrome, requiring rapid and effective assessment, diagnosis and treatment if the best possible outcome for the patient is to be achieved. Assessment and diagnosis should be undertaken as an emergency. Surgery, when it is required, must be performed at the earliest opportunity. Nevertheless, despite optimal medical care, many patients with CES will suffer long-term symptoms with significant disability, which is often hidden for the rest of their lives.
- Those at risk (see above) who do not have a cauda equina syndrome but who are at high risk should have an urgent MRI. If there is a large central disc prolapse, they should have urgent surgery to prevent the development of cauda equina syndrome.
- In reality few of those referred to as CES will need emergency surgery but escalate all for an expert opinion.
- Those with CES need urgent MRI and consult with the Spinal team with a plan for surgery within 48 hrs of onset. Laminectomy and decompression where possible
- Spinal neurorehabilitation may be possible with work on bowel and bladder and mobility and mobility aids depending on lasting neurological damage
References
- Greenhalgh, S and Finucane, L and Mercer, C and Selfe, James (2018) Assessment and management of cauda equina syndrome. Musculoskeletal Science and Practice, 37. pp. 69-74. ISSN 2468-7812
- Standards of Care for Investigation and Management of Cauda Equina Syndrome
- An Algorithm for Suspected Cauda Equina Syndrome NV Todd