Makindo Medical Notes.com |
|
|---|---|
| Download all this content in the Apps now Android App and Apple iPhone/Pad App | |
| MEDICAL DISCLAIMER:The contents are under continuing development and improvements and despite all efforts may contain errors of omission or fact. This is not to be used for the assessment, diagnosis or management of patients. It should not be regarded as medical advice by healthcare workers or laypeople. It is for educational purposes only. Please adhere to your local protocols. Use the BNF for drug information. If you are unwell please seek urgent healthcare advice. If you do not accept this then please do not use the website. Makindo Ltd | |
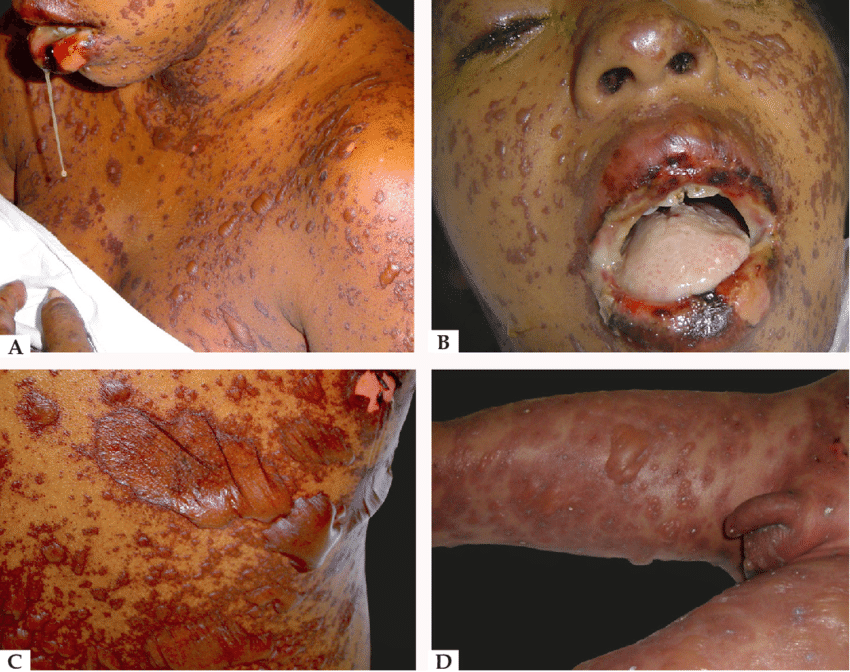
Toxic Epidermal Necrolysis (TEN)
-
| About | Anaesthetics and Critical Care | Anatomy | Biochemistry | Cardiology | Clinical Cases | CompSci | Crib | Dermatology | Differentials | Drugs | ENT | Electrocardiogram | Embryology | Emergency Medicine | Endocrinology | Ethics | Foundation Doctors | Gastroenterology | General Information | General Practice | Genetics | Geriatric Medicine | Guidelines | Haematology | Hepatology | Immunology | Infectious Diseases | Infographic | Investigations | Lists | Microbiology | Miscellaneous | Nephrology | Neuroanatomy | Neurology | Nutrition | OSCE | Obstetrics Gynaecology | Oncology | Ophthalmology | Oral Medicine and Dentistry | Paediatrics | Palliative | Pathology | Pharmacology | Physiology | Procedures | Psychiatry | Radiology | Respiratory | Resuscitation | Rheumatology | Statistics and Research | Stroke | Surgery | Toxicology | Trauma and Orthopaedics | Twitter | Urology
Related Subjects: |Nikolsky's sign |Koebner phenomenon |Erythema Multiforme |Pyoderma gangrenosum |Erythema Nodosum |Dermatitis Herpetiformis |Lichen Planus |Acanthosis Nigricans |Acne Rosacea |Acne Vulgaris |Alopecia |Vitiligo |Urticaria |Basal Cell Carcinoma |Malignant Melanoma |Squamous Cell Carcinoma |Mycosis Fungoides (Sezary Syndrome) |Xeroderma pigmentosum |Bullous Pemphigoid |Pemphigus Vulgaris |Seborrheic Dermatitis |Pityriasis/Tinea versicolor infections |Pityriasis rosea |Scabies |Dermatomyositis |Toxic Epidermal Necrolysis |Stevens-Johnson Syndrome |Atopic Eczema/Atopic Dermatitis |Psoriasis
Toxic Epidermal Necrolysis (TEN) is a rare cause of life-threatening dermatological failure. It is at the most severe end of an overlapping spectrum of disease encompassing Stevens- Johnsons syndrome. The mechanism is thought to involve an immune mediated reaction against the adhesion molecules between the epidermal and dermal layers.
About
- Likely the same disease as Stevens-Johnson syndrome but more severe
- Exfoliation with sheets of epidermal detachment
Aetiology
- Idiopathic - worse prognosis than drug-induced, Leukaemia, lymphoma
- Drug induced - sulphonamides, cephalosporins, antibiotics, anticonvulsants e.g. carbamazepine
- Commoner with HIV and other viral infections
- Commoner in slow acetylators
Drugs causing 50% of case
- Allopurinol
- Carbamazepine
- Lamotrigine
- Nevirapine
- Oxicam NSAIDs
- Phenobarbital
- Phenytoin
- Sulfamethoxazole and other sulfur agents
- Sulfasalazine
Clinical
- Preceding flu-like illness with myalgia, fever
- Spreading tender erythema and confluent blistering rash
- Involves skin and mucosa - mouth, conjunctiva, genitals
- Detachment of the epidermis and mucous membranes
- Progressive exfoliation and possible sepsis and/or death
Differential diagnosis
- Staphylococcal scalded skin syndrome (SSS) (mucosa spared)
- Toxic shock syndrome
- Phototoxic skin reactions
- Drug reaction with eosinophilia
SCORTEN Severity score
- Age > 40 years +1
- Heart rate >120 beats per minute +1
- Cancer or haematologic malignancy +1
- Involved body surface area >10% +1
- Blood urea nitrogen level >10 mmol/L (28 mg/dL) +1
- Serum bicarbonate level < 20 mmol/L (20 mEq/L) +1
- Blood glucose level > 14 mmol/L (252 mg/dL) +1
Mortality rates based on the number of positive criteria are as follows
- 0 to 1 factor = 3%
- 2 factors = 12%
- 3 factors = 35%
- 4 factors = 58%
- 5 or more factors = 90%
Investigations
- FBC, U&E, LFT, CRP
- Skin biopsy to differentiate TEN from SSS
- Blood cultures, Urine culture, CXR if febrile
Management
- Patients transferred from other hospitals for specialised management who have a SCORTEN score of 2 or more should be admitted to the Critical care unit for assessment.
- Patients with >10% body surface area (BSA) involvement or those unable to have healthcare needs met at level 1/ward based care should be discussed with critical care.
- Ensure the presence of CO₂ fire extinguishers and fire blanket are available at the patient bedside given the highly flammable nature of the treatment
- Generally supportive - fluid balance and nutrition, avoid hypothermia
- Resuscitation: includes the use of manual paddles for defibrillation. On admission of a TEN patient to critical care the resus team should be informed and defibrillation paddles obtained from medical high care. In the event that the patient requires cardiopulmonary resuscitation (CPR), use a towel and remove as much of the emollient cream as possible. Defibrillator paddles must be used in the need for DC shock. The paddles can be obtained from MHCU and should be obtained on the admission of the patient to ICU. Extreme care must be taken as the creams are highly flammable If cardioversion is required a CO₂ extinguisher and fire blanket should be available at the bedside as per the admission checklist
- AIRWAY: Any potential airway compromise mandates that the initial intubation should take place within a theatre environment with anaesthetic support. Airway compromise can come from mucosal blistering or life-threatening haemorrhage from mucosal disease, both of which have been reported in the literature. A sub-glottic suction ETT should be sited if possible. Non-adhesive tapes should be used for the fixation of endotracheal or nasogastric tubes to minimise further epidermal losses. The ventilator acquired pneumonia ( VAP) care bundle should be adhered to as per unit policy
- BREATHING:TEN patients are considered high risk for Acute Lung Injury/Acute Respiratory Distress Syndrome (ALI/ARDS) and as such the suggested initial ventilation strategy includes: Ventilate 6-8ml/kg Ideal Body Weight. Plateau pressures <30cmH₂O. Bedside PEEP titration by senior
- CIRCULATION: IV access and invasive monitoring should be established through unaffected skin if possible but if necessary it can be sited through an affected area. The use of ECG dots should be avoided to stop any further skin damage. All invasive lines should be sutured into place and dressed with Chlorhexidine impregnated dressings with the adhesive area trimmed to a minimum. The fluid requirements are less than those seen in thermal injuries but may be considerable in the acute phase. The endpoints for fluid resuscitation should be: lactate <2.0 mmol/l, 0.5-1.0ml/kg/hr urine. Overaggressive crystalloid use increases extravascular lung water and may potentiate other organ dysfunction
- Serum Albumin should be maintained >25g/l using 4.5% Albumin solution if the patient is hypovolemic and 20% Human Albumin Solution if euvolemic. Transfusion of blood and blood products may be indicated to maintain Hb >70 or >90 g/dl in the presence of cardiovascular disease. A cross-matched blood sample should be present in the lab 24/7 during ICU admission as blood loss at dressing changes, generalised oozing from the dermis or nasopharyngeal haemorrhage can be expected. Coagulopathy is common, the treatment is supportive. Cardiovascular support using vasopressors and inotropes should be guided by flow monitoring if practically possible. (Oesophageal Doppler may be contraindicated in the presence of oropharyngeal involvement and ECHO impractical in the presence of precordial epidermal loss).
- DISABILITY: Effective analgesia is of paramount importance and dressing changes may necessitate deep sedation with anxiolytic agents, such as: Fentanyl lollypops, Opiate boluses, Entonox (can be obtained via the pain team), Ketamine, Midazolam. Analgesia and/or conscious sedation should only be administered by a competent practitioner. Consider early referral to the pain team. Longer-acting Adjunctive medications may be required such as gabapentin.
- EXPOSURE: Core temperature should be monitored using a rectal probe or catheter with thermistor, peripheral temperature should be measured by any practical means, the presence of a core to peripheral temperature gradient >2°C should be managed aggressively. Moderate hyperthermia 38-38.5°C can be expected as a part of the disease process. Hypothermia should be prevented by warming the side room to 25-28°C using a portable heater. Forced air warmers, e.g. Bair Hugger, will damage broken (but replaced protective epidermal layers) and should not be used. Blood products and resuscitation fluids should be actively warmed using a warming coil. A humidified ventilator circuit should be considered. Patients should be nursed on air loss mattress (see nursing guidance for further information)
- FEEDING: Enteral feeding should be instituted once the nasogastric tube position has been confirmed on CXR. This must be secured with a bridle. Supplemental parenteral nutrition should be considered early to meet energy and protein goals. All patients will require a dietician review. Prior to this review, the provisional goals are: 25-30kcal/kg/day – dry ideal body weight.2g/kg/day protein minimum, Forceval once-daily vitamin supplement. Glycaemic control utilising critical care protocol Many TEN patients will have had inadequate enteral intake for 5-7 days and are at risk of refeeding syndrome. Electrolyte abnormalities should be expected and both Mg²⁺ and PO4
- INFECTION: The prevention of nosocomial infection is of paramount importance and standard ICU care is indicated including: Strict barrier nursing should be ensured Use of prontoderm for MRSA prophylaxis should be discussed with the dermatology team. Chlorhexidine dental gel and mouthwashes – even in the presence of mucosal injury. 2-hourly sub-glottic suction ? PPE during patient contact - apron and gloves for all patient contact & standard visor/facemask for airway interventions. Vigilance for signs of catheter-related line infection. If there is suspicion of a line infection then peripheral cultures should be sent with paired CVC cultures. If the surrounding skin is red or there is pus at the entry site the line should be removed and a new line sited. Daily surveillance of skin wound swabs should be undertaken. All patients are at high risk of MRSA acquisition. It is important to be aware that during the various phases of TEN, the exposed dermis is susceptible to microbial colonisation. Initially by Staphylococcus aureus and later by gram-negative rods from the digestive flora, especially Pseudomonas aeruginosa. A cutaneous infection will impair re-epithelialisation and may lead to systemic sepsis, which is the commonest cause of death in TEN. Indiscriminate administration of prophylactic systemic antibiotics may increase skin colonisation, particularly with Candida albicans, therefore antimicrobial therapy should only be instituted if there are clinical signs of infection. This should always be discussed as part of the daily MDT assessments with the Dermatology team. The TEN disease process may be accompanied by fever and therefore diagnosis of secondary infection may be complicated. It is important to look for other signs of systemic infection such as confusion, hypotension, reduced urine output and reduced oxygen. An increase in skin pain can be evident of cutaneous infection. Consider activation of Herpes Simplex Virus ( HSV) in eroded or vesicular areas which are slow to heal, particularly in genital or oral sites
- EYE CARE: Aim is to promote skin healing and prevent complications such as Symblepharon which is the formation of fibrous tracts that tether the bulbar to the conjunctival epithelium of the eyeball. Check that the patient is referred to the ophthalmology team. Administration of eye drops/ointment as prescribed. Gentle handling of the eyelids to prevent skin loss, use of cotton bud sticks may be required to lift the eyelids
References
Images