Related Subjects:
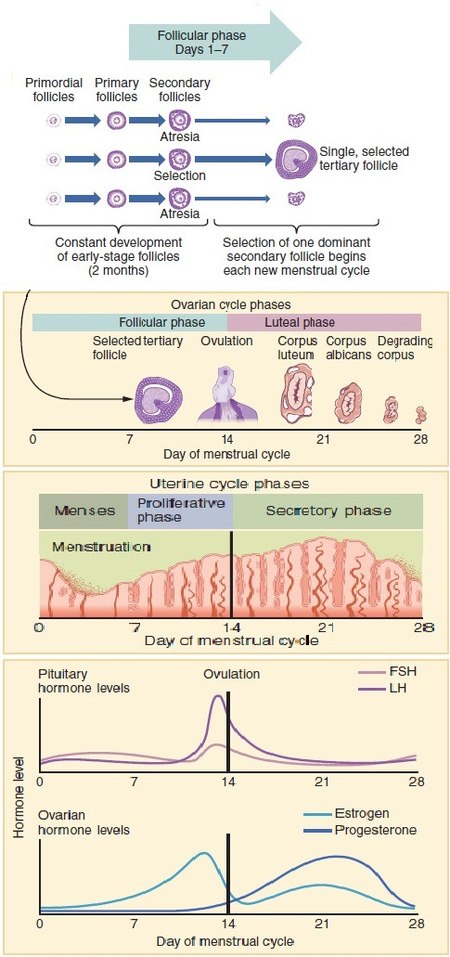
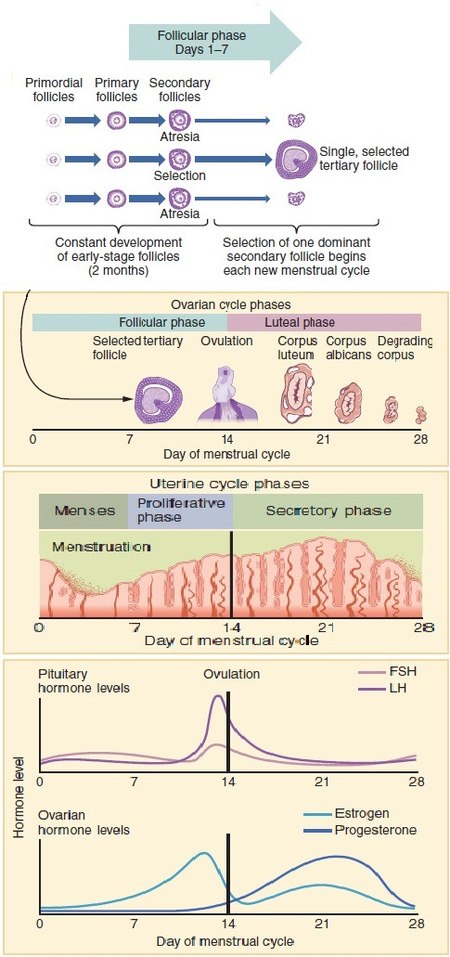
Overview of the Menstrual Cycle
The menstrual cycle is a regular natural change that occurs in the female reproductive system, specifically the uterus and ovaries, that makes pregnancy possible. It is divided into several phases, each characterized by specific hormonal and physiological changes. The average menstrual cycle lasts about 28 days, but it can range from 21 to 35 days in adults.
Phases of the Menstrual Cycle
- Menstrual Phase:
- Days 1-5
- The menstrual phase marks the beginning of the cycle and involves the shedding of the endometrial lining of the uterus, resulting in menstrual bleeding.
- Triggered by the decline in estrogen and progesterone levels at the end of the previous cycle.
- Follicular Phase:
- Days 1-13 (overlaps with the menstrual phase in the first few days)
- Characterized by the growth and maturation of ovarian follicles under the influence of follicle-stimulating hormone (FSH).
- Estrogen levels begin to rise as the follicles develop, leading to the thickening of the endometrial lining.
- Ends with a surge in luteinizing hormone (LH) that triggers ovulation.
- Ovulation:
- Day 14 (approximately)
- Ovulation is the release of a mature egg from the dominant follicle in the ovary.
- Triggered by a peak in LH and FSH levels.
- The egg travels down the fallopian tube towards the uterus, where it may meet sperm and become fertilized.
- Luteal Phase:
- Days 15-28
- After ovulation, the ruptured follicle transforms into the corpus luteum, which secretes progesterone and some estrogen.
- Progesterone prepares the endometrium for potential implantation of a fertilized egg by thickening and maintaining the lining.
- If fertilization does not occur, the corpus luteum degenerates, leading to a drop in progesterone and estrogen levels.
- The decline in these hormones triggers the start of the menstrual phase, beginning the cycle anew.
Hormonal Regulation
- Gonadotropin-Releasing Hormone (GnRH):
- Secreted by the hypothalamus in a pulsatile manner.
- Stimulates the anterior pituitary to release FSH and LH.
- Follicle-Stimulating Hormone (FSH):
- Promotes the growth and maturation of ovarian follicles.
- Stimulates the production of estrogen by the granulosa cells of the follicles.
- Luteinizing Hormone (LH):
- Triggers ovulation and the formation of the corpus luteum.
- Stimulates the production of progesterone by the corpus luteum.
- Estrogen:
- Produced by the developing follicles and the corpus luteum.
- Stimulates the proliferation and thickening of the endometrial lining.
- Regulates the release of GnRH, FSH, and LH through feedback mechanisms.
- Progesterone:
- Produced by the corpus luteum after ovulation.
- Maintains the endometrial lining for potential implantation of a fertilized egg.
- Inhibits the release of GnRH, FSH, and LH to prevent further ovulation within the same cycle.
Physiological Changes
- Endometrium:
- Undergoes cyclic changes in response to hormonal fluctuations.
- Proliferative phase: Thickening of the endometrium under the influence of estrogen during the follicular phase.
- Secretory phase: Further preparation of the endometrium under the influence of progesterone during the luteal phase.
- Menstrual phase: Shedding of the endometrial lining if fertilization does not occur.
- Cervical Mucus:
- Changes in consistency and quantity throughout the cycle.
- During the follicular phase, estrogen makes the mucus thin and slippery to facilitate sperm passage.
- During the luteal phase, progesterone makes the mucus thick and less permeable to sperm.
- Basal Body Temperature:
- Increases slightly after ovulation due to the thermogenic effect of progesterone.
- Tracking basal body temperature can help identify ovulation and fertile windows.
Clinical Relevance
- Menstrual Disorders:
- Amenorrhea: Absence of menstruation.
- Dysmenorrhea: Painful menstruation.
- Menorrhagia: Heavy menstrual bleeding.
- Irregular menstruation: Variation in cycle length and flow.
- Hormonal Contraception:
- Utilizes synthetic hormones to prevent ovulation, alter cervical mucus, and change the endometrial lining to prevent pregnancy.
- Fertility Awareness:
- Methods based on tracking menstrual cycle changes to identify fertile and infertile phases for family planning purposes.
Summary
The menstrual cycle is a complex process regulated by hormonal interactions that prepare the female body for potential pregnancy. It involves cyclical changes in the ovaries and endometrium, driven by the coordinated actions of GnRH, FSH, LH, estrogen, and progesterone. Understanding the physiology of the menstrual cycle is essential for managing reproductive health, diagnosing menstrual disorders, and utilizing fertility awareness methods.