Makindo Medical Notes.com |
|
|---|---|
| Download all this content in the Apps now Android App and Apple iPhone/Pad App | |
| MEDICAL DISCLAIMER:The contents are under continuing development and improvements and despite all efforts may contain errors of omission or fact. This is not to be used for the assessment, diagnosis or management of patients. It should not be regarded as medical advice by healthcare workers or laypeople. It is for educational purposes only. Please adhere to your local protocols. Use the BNF for drug information. If you are unwell please seek urgent healthcare advice. If you do not accept this then please do not use the website. Makindo Ltd | |
Aortic Dissection
-
| About | Anaesthetics and Critical Care | Anatomy | Biochemistry | Cardiology | Clinical Cases | CompSci | Crib | Dermatology | Differentials | Drugs | ENT | Electrocardiogram | Embryology | Emergency Medicine | Endocrinology | Ethics | Foundation Doctors | Gastroenterology | General Information | General Practice | Genetics | Geriatric Medicine | Guidelines | Haematology | Hepatology | Immunology | Infectious Diseases | Infographic | Investigations | Lists | Microbiology | Miscellaneous | Nephrology | Neuroanatomy | Neurology | Nutrition | OSCE | Obstetrics Gynaecology | Oncology | Ophthalmology | Oral Medicine and Dentistry | Paediatrics | Palliative | Pathology | Pharmacology | Physiology | Procedures | Psychiatry | Radiology | Respiratory | Resuscitation | Rheumatology | Statistics and Research | Stroke | Surgery | Toxicology | Trauma and Orthopaedics | Twitter | Urology
Related Subjects: |Assessing Chest Pain |Acute Coronary Syndrome (ACS) General |Aortic Dissection |Pulmonary Embolism |Acute Pericarditis |Diffuse Oesophageal Spasm |Gastro- oesophageal reflux |Oesophageal Perforation Rupture |Pericardial Effusion Tamponade |Pneumothorax |Tension Pneumothorax |Shingles
The most important action is considering the diagnosis in a patient with chest pain and not misdiagnosing it as the far commoner MI or PE. Acute anticoagulation treatment for PE or MI is unhelpful in dissection with a risk of bleeding which will need imminent surgery.
Tearing, stabbing rip
Intima has lost its grip
Swift rift prunes each branch
Wide aortic silhouette
CT now to detail threat
@DrCindyCooper
| Management of Acute Aortic Dissection |
|---|
|
A potential cause of late pregnancy and post partum chest pain or cardiac arrest along with PE. POCUS may be very helpful.
About
- Approximately 40% are initially fatal and 10% die during or immediately after surgery.
- If suspected then urgent CT and if Type A dissection found you must reduce BP
- Type A need to get the patient to a cardiothoracic centre
- The constant systolic pressure wave dp/dt needs reduced with beta blockade
- Very rarely Aortic dissection can be a chronic condition over several weeks
Aortic anatomy
Aetiology
In younger patients there are associated connective tissue disorders, whilst older patients are more likely to have underlying hypertension or atherosclerosis.
- The aorta consists of the layers intima, media and adventitia.
- A dissection occurs when bleeding occurs into the media of the thoracic or abdominal aorta.
- There is usually an associated intimal tear and flap.
- There is formation of a true and false lumen
- Associated with hypertension and connective tissue disease
- Intimal tears happen in two common places
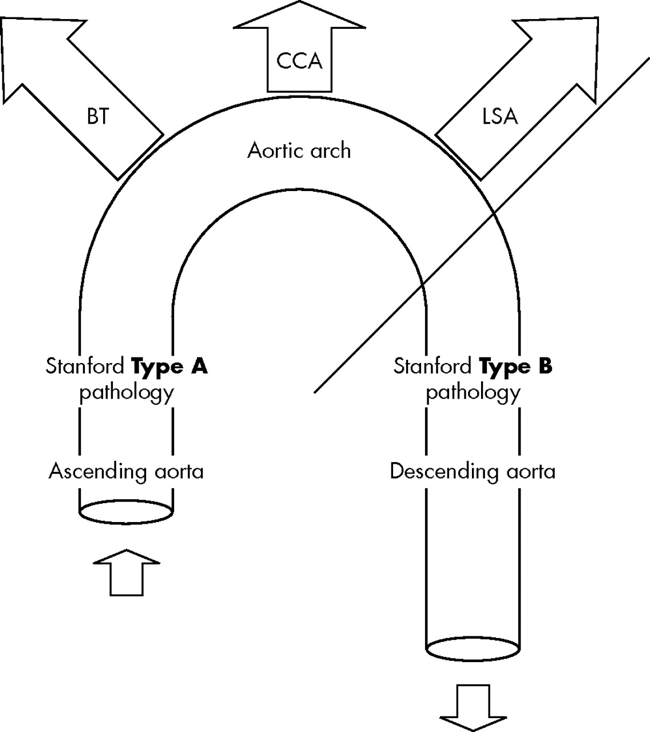
- 1. Within a few centimetres of the aortic valve and these are Type A dissections
- 2. Just distal to left subclavian artery and these become Type B dissections
- Dissections can proceed in one or more directions
- Antegrade towards the aortic arch and beyond causing damage to the aortic arch and distal branches
- Retrograde back to aortic valve causing tamponade, aortic regurgitation or coronary ostial damage
- Out of the aorta - rupture which can cause a left pleural effusion and death
- Back into the lumen - very lucky
Risks
- Men > women, Hypertension
- Atherosclerotic aorta
- Coarctation of the aorta
- Cystic medial degeneration
- Marfan's disease, Ehlers-Danlos syndrome
- Previous surgery e.g. CABG, AVR,
- Trauma, bicuspid aortic valves,
- Cocaine use, Pregnancy (3rd trimester)
- Connective tissue disease, Aortitis.
Stanford classification
- Type A: Commoner causing 2/3rd of cases. Proximal to the Left subclavian which require urgent BP lowering and cardiothoracic surgery. Intimal flaps occur most often within a few cms of the aortic valve.
- Type B: Distal to the left subclavian which is managed medically through blood pressure control. Intimal flaps are seen just distal to left subclavian vessel and can extend all the way down to the iliacs.
 VF
VF

DeBakey Classification
- Type I: originates in the ascending aorta and propagates at least to the aortic arch. Usually patient < 65. Highest mortality. 1% per hour
- Type II: confined to the ascending aorta. Elderly patients. Atherosclerosis and HTN
- Type III: distal to the subclavian artery in the descending aorta
Complications
- Type A Proximal
- Aortic rupture and sudden death
- Stroke and ischaemic arms and loss of pulse due to shearing off of the origin of head and neck vessels
- Acute Aortic regurgitation
- Myocardial infarction (RCA) if coronary vessels involved.
- Type B Distal
- Spinal cord infarction with distal dissection affecting supply to cord- "Spinal stroke"
- Mesenteric/renal ischaemia
- Left pleural haemothorax - ominous sign on CXR suggesting haemorrhage
Associations
- Hypertension, Aortic atherosclerosis, Cystic medial degeneration
- Marfan's syndrome, Ehlers-Danlos syndrome, Noonan's syndrome, Turner's syndrome
- Trauma, Cocaine, Pregnancy - a cause of sudden death
- Coarctation of the Aorta, Bicuspid aortic valves +/- stenosis
- Aortitis - Takayasu's, Syphilis, Giant cell arteritis
Clinical: Disparities in BP are normal and seen in 20% of patients
- May mimic a MI/ACS and patients may get ACS management which can be harmful
- Suspect in any patient with sharp, ripping, chest pain especially with radiation into the back.
- Patients look shocked but often hypertensive with tearing interscapular pain
- Murmur over left scapula may be heard
- Patient may be hypertensive or alternatively shocked if there is blood loss
- Chest pain due to MI as coronary artery (usually RCA) involved
- There may be a difference in pulse and BP in each arm.
- Dissection may shear of vessels in the proximal aorta
- Look for the murmur of aortic regurgitation and resultant pulmonary oedema
- Syncope was reported in 15% of patients
Effects by vessel occluded
- Coronary artery: STEMI usually RCA with Inferior MI as Left coronary occlusion usually instantly fatal
- Common Carotid artery: Ipsilateral Anterior circulation infarct
- Subclavian artery: Posterior circulation stroke - ataxia, brainstem and visual signs, Cold upper limb, Delayed pulse
- Anterior spinal artery: bilateral leg weakness and paraplegia, dorsal columns intact
- Renal arteries: AKI, Oliguria. Coeliac artery: Gut ischaemia
Differential
- Acute coronary syndrome
- Acute Pericarditis
- Pneumothorax
- Pulmonary Embolism
Aortic Dissection Detection Risk Score (ADD-RS)
- Use with caution as not fully validated
- Low to moderate risk patients for whom acute aortic syndromes are in the differential diagnosis.
- Aortic Dissection Detection Risk Score
- May require the additional use of Dimer prior to decision to do CTA
Investigations
- U&E, FBC, LFTs, Group and cross match in tertiary centre for surgery
- CXR: Unfolded aorta, widening of the mediastinum, left pleural effusion could be a sign of haemothorax.
- ECG: Any arrhythmias. Inferior MI if RCA is involved. Death if LMS involved
- D-Dimer: often very elevated so a normal level might be useful for excluding dissection
- Troponin: may be elevated
- Transthoracic Echo: suprasternal views may be useful and may be done in unstable patients preoperatively but not as useful as TOE/TEE
- Trans oesophageal echo (TEE/TOE) if available: may show dissection may be done in unstable patients preoperatively and shows dynamic changes and flow to branches
- CT Aortogram/Thorax - most practical and shows true and false lumen of dissection. Can be done prior to surgery if stable enough. The true lumen is usually round or oval and has a strong doppler velocity and thrombus is rare. The false lumen is crescentic and usually has poor doppler flow and thrombus is common
Complications
- Aortic rupture due to breakdown in intima and media
- Stroke if carotids involved
- Cardiac tamponade.
- Acute Aortic regurgitation
- Spinal cord infarction and paraparesis
- Mesenteric/renal ischaemia
- Left pleural haemothorax - ominous sign on CXR
- Sudden death
Management
- ABC, Good IV access. Resuscitation. Many patients are hypertensive. Treat chest pain IV Diamorphine 2.5-5 mg or Morphine 5-10 mg. Close monitoring. Confirm suspected aortic dissection with CT Aortogram and/or TOE/TEE and avoid any anticoagulation or anti-platelets or thrombolysis
- If Type A proximal dissection is found then urgently manage BP and discuss with the cardiothoracic centre for advice and transfer. Type A AD has a mortality of 50% within the first 48 hours if not operated. Despite improvements in surgical and anaesthetic techniques, perioperative mortality (25%) and neurological complications (18%) remain high. The urgent transfer is indicated and time to surgery mirrors mortality.
- In meantime reduce Blood pressure and pulse pressure to reduce the dp/dt that is driving the dissection. Usually, IV Labetalol 30-50 mg IV. Also consider Nitroprusside. Some studies have shown that emergency pericardiocentesis of an acute Type A aortic dissection complicated by cardiac tamponade can result in deterioration and should be avoided if possible and every effort should be made to proceed as urgently as possible to the operating room for direct surgical repair of the Aorta with intraoperative drainage of the haemopericardium.
- Open Surgical repair is the standard for Type A: this has much higher mortality and is now rare. Surgeons replace the proximal aorta with a tube graft. Consider new aortic valve and sewing in coronary vessels.
- BP control and Endovascular treatment is now the standard for Type B by the closure of dissection with an endovascular stent passed via the femoral artery. This compresses the dissection and redirects blood across the true lumen.
- Type B dissections have a much lower risk of complications so are usually managed medically and conservatively using medical therapy to reduce BP with Beta blockade - IV Labetalol and Nitroprusside often used.