Makindo Medical Notes.com |
|
|---|---|
| Download all this content in the Apps now Android App and Apple iPhone/Pad App | |
| MEDICAL DISCLAIMER:The contents are under continuing development and improvements and despite all efforts may contain errors of omission or fact. This is not to be used for the assessment, diagnosis or management of patients. It should not be regarded as medical advice by healthcare workers or laypeople. It is for educational purposes only. Please adhere to your local protocols. Use the BNF for drug information. If you are unwell please seek urgent healthcare advice. If you do not accept this then please do not use the website. Makindo Ltd | |
Lower Gastrointestinal (Rectal) Bleeding
-
| About | Anaesthetics and Critical Care | Anatomy | Biochemistry | Cardiology | Clinical Cases | CompSci | Crib | Dermatology | Differentials | Drugs | ENT | Electrocardiogram | Embryology | Emergency Medicine | Endocrinology | Ethics | Foundation Doctors | Gastroenterology | General Information | General Practice | Genetics | Geriatric Medicine | Guidelines | Haematology | Hepatology | Immunology | Infectious Diseases | Infographic | Investigations | Lists | Microbiology | Miscellaneous | Nephrology | Neuroanatomy | Neurology | Nutrition | OSCE | Obstetrics Gynaecology | Oncology | Ophthalmology | Oral Medicine and Dentistry | Paediatrics | Palliative | Pathology | Pharmacology | Physiology | Procedures | Psychiatry | Radiology | Respiratory | Resuscitation | Rheumatology | Statistics and Research | Stroke | Surgery | Toxicology | Trauma and Orthopaedics | Twitter | Urology
Related Subjects: |Ulcerative Colitis |Microscopic colitis |Irritable bowel syndrome |Lower Gastrointestinal (Rectal) Bleeding
PR bleeding of fresh blood within the first 24 h of hospitalization with a drop in the haemoglobin of at least 2 g/dL and/or a transfusion requirement of at least 2 units of packed red blood cells, urgent diagnosis and intervention are required to control the bleeding.
| Lower Gastrointestinal (Rectal) Bleeding |
|---|
|
About
- Bleeding from the GI tract from beyond the Ligament of Treitz.
- In practice is predominantly Colorectal.
- More common in the elderly and anticoagulated
- If unsure then OGD and capsule endoscopy should also be considered
- Overall mortality rate from colonic bleeding is 2.4-3.9 %
Risks for severe bleeding
- Aspirin use
- Two or more comorbid illnesses
- Pulse greater than 100/minute
- Systolic blood pressure <115 mmHg
- Age over 70 years
- Intestinal ischaemia
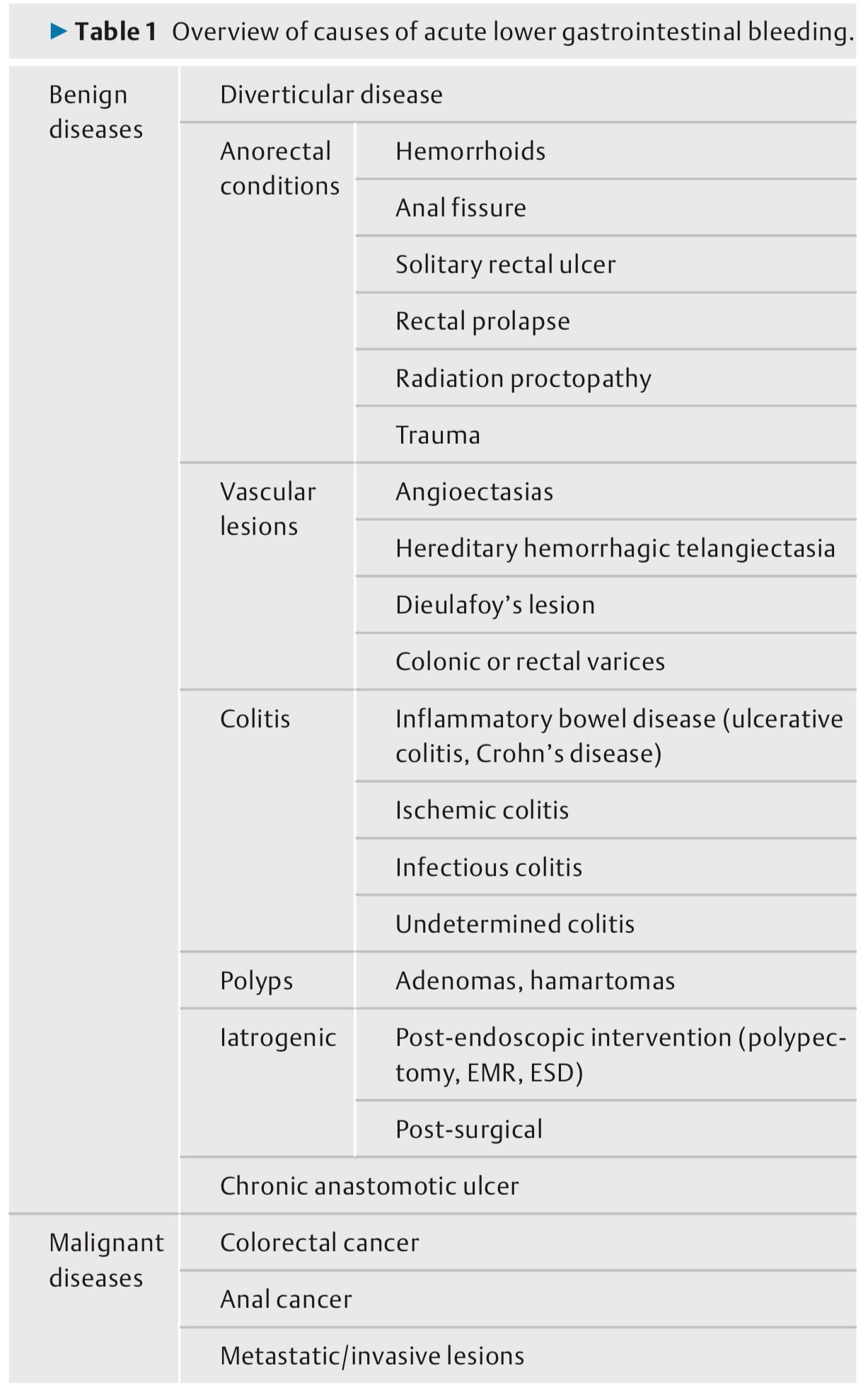
Aetiology
- Diverticular disease 35%
- Inflammatory bowel disease 15%
- Colonic polyp or Colorectal cancer 15%
- Angiodysplasia 10%
- Ischaemic colitis
- Pseudomembranous colitis
- Meckel's diverticulum
- Haemorrhoids
Haematochezia (PR bleeding) associated with haemodynamic instability may be a large upper gastrointestinal (GI) bleeding source and thus warrants an OGD (EGD) to check the top end.
Clinical
Investigations
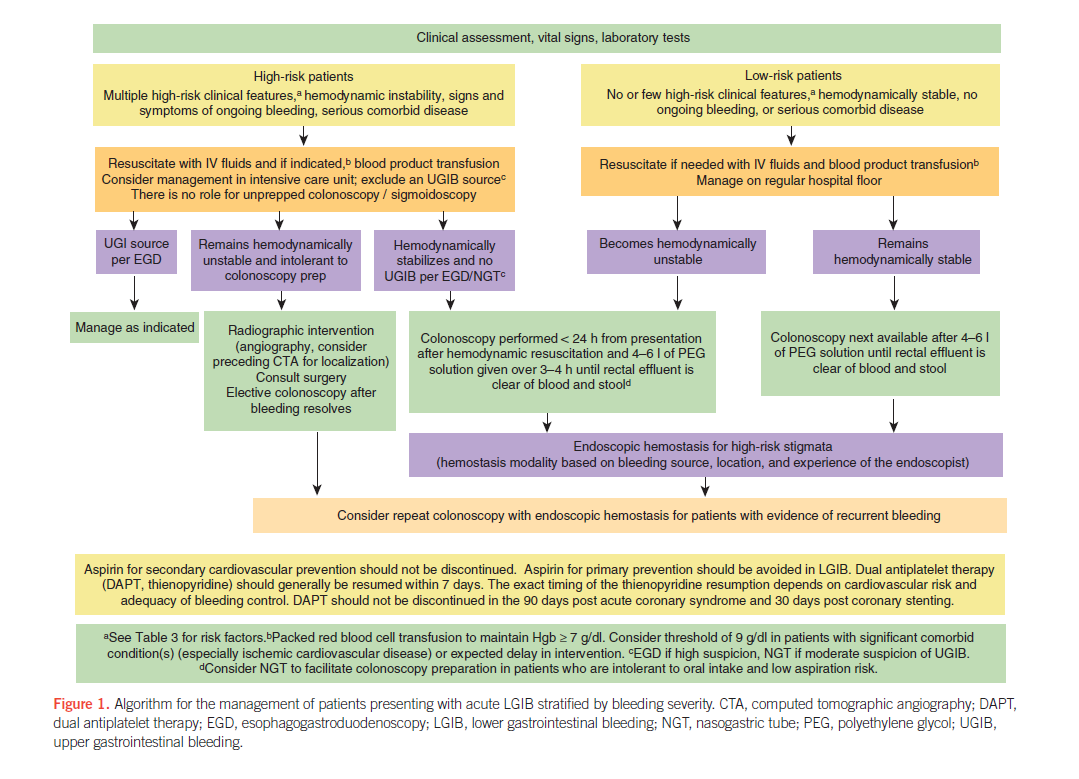
ACG Clinical Guideline: Management of Patients with Acute Lower Gastrointestinal Bleeding 2016
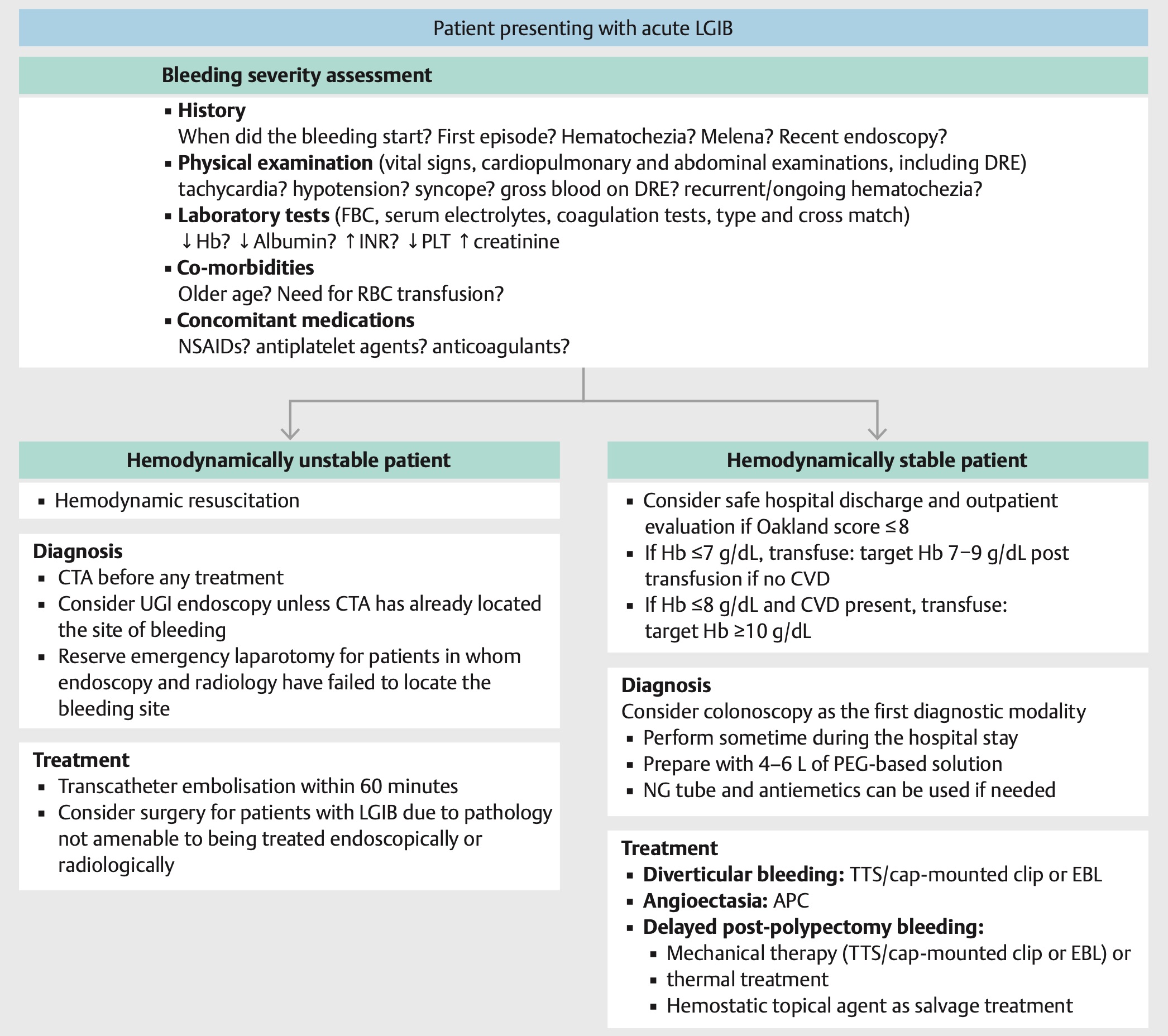
Another Algorithm
Management
References