Makindo Medical Notes.com |
|
|---|---|
| Download all this content in the Apps now Android App and Apple iPhone/Pad App | |
| MEDICAL DISCLAIMER:The contents are under continuing development and improvements and despite all efforts may contain errors of omission or fact. This is not to be used for the assessment, diagnosis or management of patients. It should not be regarded as medical advice by healthcare workers or laypeople. It is for educational purposes only. Please adhere to your local protocols. Use the BNF for drug information. If you are unwell please seek urgent healthcare advice. If you do not accept this then please do not use the website. Makindo Ltd | |
Resus: Septic Shock and Sepsis
-
| About | Anaesthetics and Critical Care | Anatomy | Biochemistry | Cardiology | Clinical Cases | CompSci | Crib | Dermatology | Differentials | Drugs | ENT | Electrocardiogram | Embryology | Emergency Medicine | Endocrinology | Ethics | Foundation Doctors | Gastroenterology | General Information | General Practice | Genetics | Geriatric Medicine | Guidelines | Haematology | Hepatology | Immunology | Infectious Diseases | Infographic | Investigations | Lists | Microbiology | Miscellaneous | Nephrology | Neuroanatomy | Neurology | Nutrition | OSCE | Obstetrics Gynaecology | Oncology | Ophthalmology | Oral Medicine and Dentistry | Paediatrics | Palliative | Pathology | Pharmacology | Physiology | Procedures | Psychiatry | Radiology | Respiratory | Resuscitation | Rheumatology | Statistics and Research | Stroke | Surgery | Toxicology | Trauma and Orthopaedics | Twitter | Urology
Related Subjects: Atropine |Acute Anaphylaxis |Basic Life Support |Advanced Life Support |Adrenaline/Epinephrine |Acute Hypotension |Cardiogenic shock |Distributive Shock |Hypovolaemic or Haemorrhagic Shock |Obstructive Shock |Septic Shock and Sepsis |Shock (General Assessment) |Toxic Shock Syndrome |Non invasive ventilation (NIV) |Intubation and Mechanical Ventilation |Critical illness neuromuscular weakness |Multiple Organ Dysfunction Syndrome
In sepsis large volumes of fluid may be required to replace fluid lost into tissues and a clinically important anaemia may result from haemodilution and blood transfusion may be necessary.
Algorithm
| Initial Management: O₂ target 94-98% unless scale 2 COPD. |
|---|
|
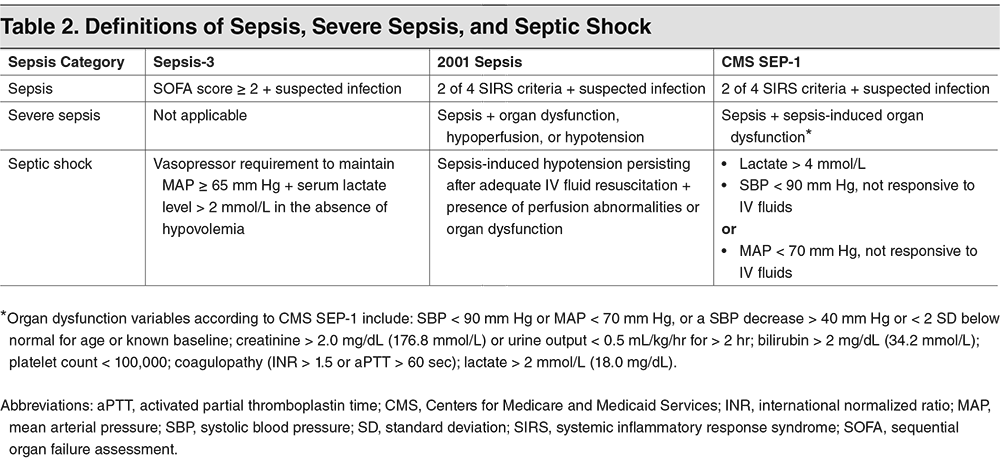
Third International Consensus (2016) Definitions
- Sepsis: "life-threatening organ dysfunction caused by a dysregulated host response to infection." In layman's terms it means that Sepsis is a self-inflicted injury due to our response to an infection.
- qSOFA (Quick SOFA) Criteria can be used to triage patients with suspected sepsis
- Respiratory rate >22/min
- Altered mentation
- Systolic blood pressure < 100 mm H
- Septic shock: sepsis with persisting hypotension requiring vasopressors to maintain MAP > 65 mm Hg and having a serum lactate level >2 mmol/L (18 mg/dL) despite adequate volume resuscitation. With these criteria, hospital mortality is in excess of 40%
Risk Factors
- Age > 75
- Impaired immunity (e.g. diabetes, steroids, chaemotherapy)
- Recent trauma / surgery / invasive procedure
- Indwelling lines / IVDU / broken skin
A metabolic acidosis with base deficit > 5 mmol/L often indicates increased lactic acid production in poorly perfused, hypoxic tissues. Serial lactate measurements may help in monitoring response to treatment
Likely Source
- Respiratory, Brain, Urine, Surgical
- Skin / joint / wound, Indwelling device, Other
Red flag sepsis: Involve Critical Care/Seniors
- Evidence of new or altered mental state
- SBP < 90 mmHg (or drop of >40 from normal)
- Heart rate > 130/minute or new AF
- Respiratory rate > 25/minute
- Needs 40% O₂ to keep SpO₂ > 92% (88% in COPD)
- Non-blanching rash / mottled / ashen / cyanotic
- Lactate > 2 mmol/l
- Recent chaemotherapy or surgery or IV Drug user
- Not passed urine in 18 hours (<0.5ml/kg/hr if catheterised)
- Mottled, ashen, or cyanotic skin. Non blanching rash
Quick SOFA: Predicts death or a requirement ICU for ward patients
- Patients are deemed positive for qSOFA if they have two of:
- Glasgow Coma Scale score of <15 (see Box 26.28 )
- Respiratory rate of = 22 breaths/min
- Systolic blood pressure of = 100 mmHg.
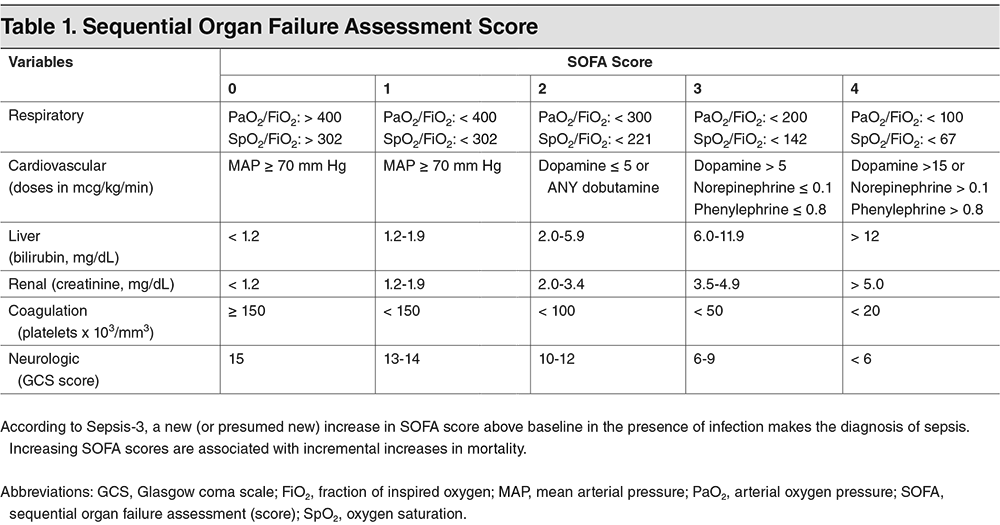
Sequential Organ Failure Assessment (SOFA) score
The SOFA score is based on six different independent scores, including respiratory, cardiovascular, hepatic, renal, coagulation, and neurological systems, and is used to check the patient's status or the extent of organ failure and dysfunction in intensive care units (ICUs). Generally, it is designed to predict mortality but not the success or failure of medical interventions.A qSOFA score of =2 is suggestive of sepsis and needs urgent review for escalation
QSOFA score
- Respiratory rate > 22/min +1
- Altered mentation GCS reduced +1
- SBP = 100 mmHg +1
Amber Flag Sepsis
- Relatives or Nursing concerns re mental state
- Acute deterioration in functional ability
- Trauma/ surgery/ procedure in last 6 weeks
- Systolic BP 91-100 mmHg (or drop >40 from normal)
- Heart rate 111- 130 per minute or new arrhythmia
- Respiratory rate 21-24 per minute or breathing hard
- Not passed urine in last 12- 18 hours
- Clinical signs of wound, device or skin infection
Microbiology
- 40% Gram positive and 60% Gram negative
- E.Coli, Staph Aureus, Streptococcus Pneumoniae
- Pyogenic streptococci e.g. Group A
- Neisseria meningitis
Coagulase negative in immunosuppressed. - Very small amount are fungal
More Definitions
- Septicaemia: SIRS + positive blood culture
- Bacteraemia: bacteria in bloodstream +/- SIRS
- Severe Sepsis: SIRS + organ dysfunction or Hypotension
- Septic shock: clinical criteria of sepsis and vasopressor therapy needed to elevate mean arterial pressure = 65 mmHg and lactate > 2 mmol/L(18mg/dL) despite adequate fluid resuscitation
Aetiology (nonspecific)
- Ischaemia, inflammation, Trauma, infection
- Several insults combined.
Aetiology
- There is reduced ability of tissues to extract Oxygen - this is a real problem with an inability to utilise oxygen for oxidative phosphorylation at the mitochondrial level
- The result being lactic acidosis and interestingly the AV O2 gap narrows as O2 is not extracted.
Severe Sepsis
- Sepsis plus at least one of the following signs of organ hypoperfusion or dysfunction
- Areas of mottled skin, capillary refilling requires three seconds or longer
- Urine output <0.5 mL/kg for at least one hour, or renal replacement therapy
- Lactate >2 mmol/L
- Abrupt change in mental status
- Abnormal electroencephalographic (EEG) findings
- Platelet count <100,000/mL
- Disseminated intravascular coagulation
- Acute lung injury or acute respiratory distress syndrome (ARDS)
- Cardiac dysfunction on echo or direct measurement of the cardiac index
Clinical
- Pyrexia, Delirium, Oliguria, Dyspnoea
- Hypotensive, Mottled skin and poor capillary return
Investigations
- FBC - WCC elevated or low, Low Hb
- U&E - renal function - possible AKI
- ↑ Amylase - pancreatitis
- CXR: consolidation, collapse, pneumothorax, malignancy
- ABG and ↑ Lactate (elevated)
- Clotting ↑ prolonged APPT and PT if DIC
- Blood and Urine cultures
- Echocardiogram - LV function, valves, tamponade, endocarditis
- Abdominal CT - perforations, obstruction, abscess, fluid collections, AAA
Monitoring
- Regular Temp, Pulse, Resp rate and O₂ saturation.
- Urinary catheter can help show renal perfusion and fluid balance
- Central venous catheter capable of measuring central venous oxygen saturation
Sepsis 6: To be completed within 1 hour
- 1. High-flow oxygen to maintain oxygen saturation >95%
- 2. Blood cultures and consider source control
- 3. Intravenous antibiotics
- 4. Intravenous fluid resuscitation
- 5. Check haemoglobin and serial lactates
- 6. Hourly urine output measurement
If after delivering the Sepsis Six, patient still has these then Refer to Intensive Care Unit
- Systolic BP <90 mmHg
- Reduced level of consciousness despite resuscitation
- Respiratory rate over 25 breaths per minute
- Lactate not reducing
- or if patient is clearly critically ill at any time
Management
- ABC, Oxygen target 94-98% unless scale 2, Good IV access.
- If in HDU/ITU central venous line and arterial line
- Give 500mL boluses of N-Saline or equivalent over 15mins. Caution in heart failure. Consider repeating if no improvement.
- Intubation and ventilation if resistant hypoxia or severe hypercapnia
- IV Broad spectrum antibiotics for the likely source. Give within 1 hour.
- If CVP < 6 mmHg then repeated bolus 250 ml N-Saline or colloid
- If CVP > 6 mmHg or poor LV suspected then 100 ml boluses
- Aim for Hb 70-90 g/L or 100 g/L if IHD
- Target mean arterial pressure (MAP) = 65 mm Hg and lactate > 2 mmol/L
- Consider Inotropes: Norepinephrine (Noradrenaline) is the Inotrope of choice and preferred to dopamine which increases arrhythmias and mortality
- Monitor haemodynamic, pH, Lactate, urine output, ABG