Makindo Medical Notes.com |
|
|---|---|
| Download all this content in the Apps now Android App and Apple iPhone/Pad App | |
| MEDICAL DISCLAIMER:The contents are under continuing development and improvements and despite all efforts may contain errors of omission or fact. This is not to be used for the assessment, diagnosis or management of patients. It should not be regarded as medical advice by healthcare workers or laypeople. It is for educational purposes only. Please adhere to your local protocols. Use the BNF for drug information. If you are unwell please seek urgent healthcare advice. If you do not accept this then please do not use the website. Makindo Ltd | |
Acute Coronary Syndrome (ACS) STEMI
-
| About | Anaesthetics and Critical Care | Anatomy | Biochemistry | Cardiology | Clinical Cases | CompSci | Crib | Dermatology | Differentials | Drugs | ENT | Electrocardiogram | Embryology | Emergency Medicine | Endocrinology | Ethics | Foundation Doctors | Gastroenterology | General Information | General Practice | Genetics | Geriatric Medicine | Guidelines | Haematology | Hepatology | Immunology | Infectious Diseases | Infographic | Investigations | Lists | Microbiology | Miscellaneous | Nephrology | Neuroanatomy | Neurology | Nutrition | OSCE | Obstetrics Gynaecology | Oncology | Ophthalmology | Oral Medicine and Dentistry | Paediatrics | Palliative | Pathology | Pharmacology | Physiology | Procedures | Psychiatry | Radiology | Respiratory | Resuscitation | Rheumatology | Statistics and Research | Stroke | Surgery | Toxicology | Trauma and Orthopaedics | Twitter | Urology
Related Subjects: |Acute Coronary Syndrome (ACS): Complications |Atherosclerosis |Ischaemic heart disease |Assessing Chest Pain |ACS - General |ACS - STEMI |ACS - NSTEMI |ACS - GRACE Score |ACS - ECG Changes |ACS -Cardiac Troponins |ACS - Post MI arrhythmias |ACS: Right Ventricular STEMI |ACS: Sgarbossa Criteria
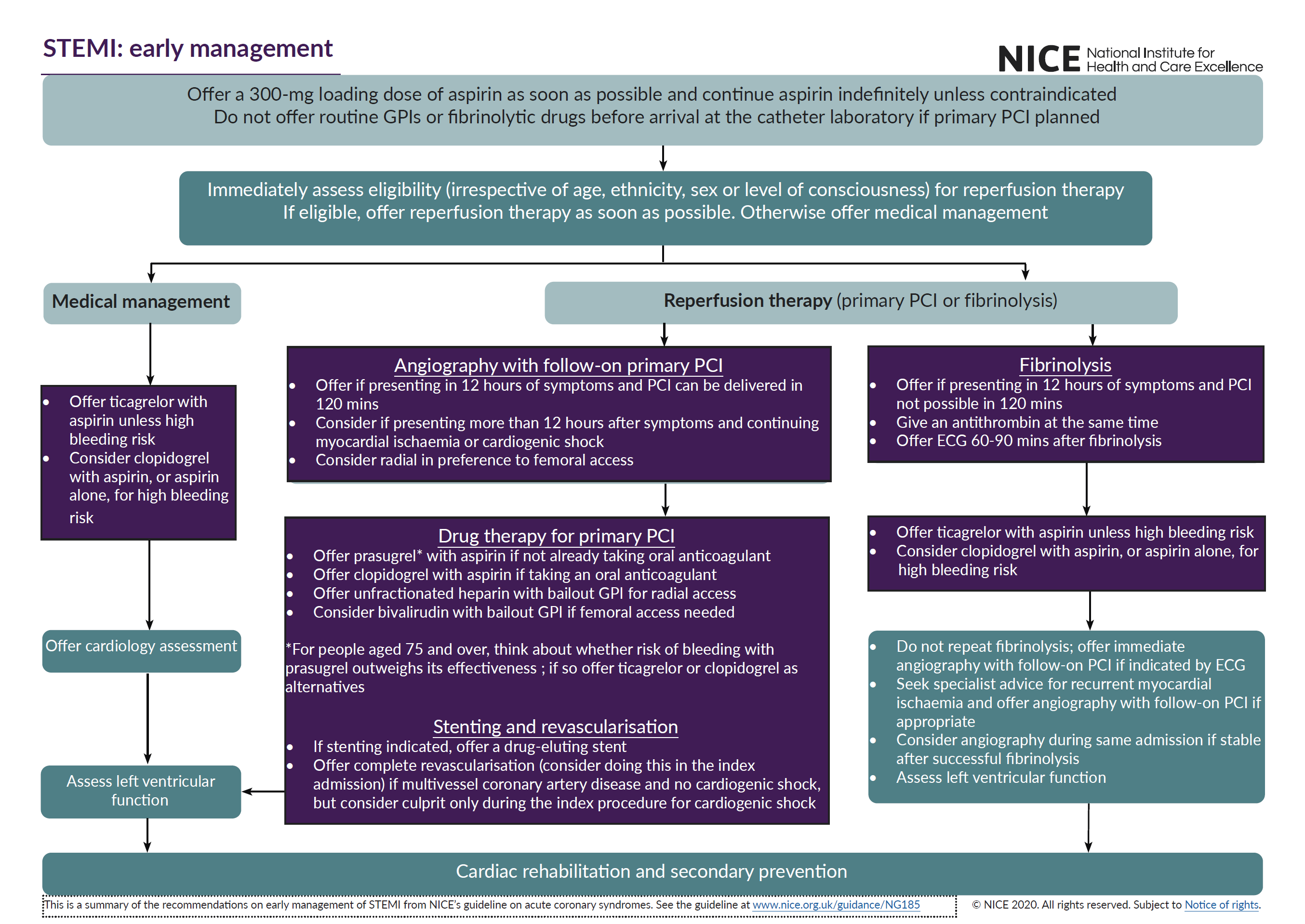
Adhere to local guidelines and expert senior cardiology advice. Always closely monitor and be ready to defibrillate. A STEMI is usually due to a complete obstruction of a coronary artery. It is important to recognise as reperfusion therapy can save lives and reduce morbidity.
| Initial Management summary for Acute STEMI |
|---|
|
Management of STEMI (Chest pain + ECG)
Refer the patient immediately to Cardiology for Primary Percutaneous Intervention (Primary PCI); the target door-balloon time is within 60 mins. Establish an IV line. Take blood samples for full blood count, U&Es, glucose, troponin, and lipids. A chest x-ray should be requested but should not delay therapy.
Aetiology
- Occluded coronary artery
- Harm depends on which artery and how proximal the lesion
- This determines how much myocardium is damaged
- Prompt treatment is very important
Clinical
- Central or retrosternal chest pain/tightness/heaviness
- Radiates to neck/shoulder/jaw
- Associated dyspnoea, nausea, vomiting
- Occasionally silent - fall, syncope with ECG changes
- Pulmonary oedema, heart block
ECG Criteria (STE = ST elevation)
- STE in two contiguous leads (1 mm = 0.1 mV)
- > 2 mm of STE in 2 contiguous V1-V6 leads in men (1.5 mm for women)
- > 1 mm in 2 other contiguous leads
- New LBBB block (Use Sgarbossa Criteria)
- RV Infarction STE in V3/V4 on Right side of chest
- Posterior MI
- A standard 12-lead ECG might not show obvious ST elevation
- Deep ST depression and tall R waves in leads V1 to V3.
- Posterior Leads (V7-V9): ST elevation, which confirms the diagnosis.
Troponin
- will be elevated at 0 and 3 hours. However, no need to wait for troponin levels if chest pain and ECG changes as above.
- If there is uncertainty and troponin not available a rapid bedside Echocardiogram may support diagnosis showing regional wall reduced motility that corresponds with ECG findings.
Actions
- NB: MI can be silent in elderly or diabetics. Ensure defibrillator available
- Clinical Assessment/NEWS/ Telemetry. IV access.
- Send FBC, U&E, LFT, Troponin and Dimer if PE/Dissection suspected
- Admit to CCU telemetry bed and at least daily Review looking for complications
Early Management and Medications
- Give Oxygen to achieve SaO₂ 94-98%
- GTN 400 mcg per spray or S/L GTN tablet (300 or 500 mcg) if Chest pain, SBP > 110 mmHg, LVF
- Pain relief: Morphine 2.5-5 mg slow IV which may be repeated as needed or Diamorphine 2.5 mg slow IV which may need repeating
- Antiemetic: Metoclopramide 10 mg IV Oxygen and Monitor
- Antiplatelet: Aspirin 300 mg PO stat
- Commence a P2Y12 antagonist: one of the following (discuss with cardiology if risk of bleeding)
- Clopidogrel 300-600 mg PO Stat
- Ticagrelor 180 mg PO stat
- Prasugrel 60 mg PO stat
- Metoprolol 5-15 mg IV or 50 mg PO BD if LV dysfunction, Tachycardia (not if Asthma or Pulmonary oedema). Alternatives are Diltiazem for those who cannot take a beta-blocker.
- Furosemide 40-80 mg IV if pulmonary oedema
- Ramipril 1.25 mg OD
- Fondaparinux 2.5 mg OD SC may be given if no reperfusion therapy
- Hyperglycaemia
- Check blood glucose on admission, and check fasting blood glucose at day 4 or HBA1C predischarge for anyone with hyperglycaemia at presentation (blood glucose >11mMol/L).
- Glucose control is important (aim BM 6-11 mmol/L), but take care to avoid hypoglycaemia (BM <4.4) which can worsen outcomes in diabetic patients with acute coronary syndromes.
- If control poor in the CCU e.g. BM > 11 mmol/L then consider starting VRII.
Reperfusion therapy if chest pain onset < 12 hrs
Primary PCI should be done within 60-90 min of admission
- Urgent transfer to Catheterisation lab if available within 90 mins of call. . Access via radial artery if it can be done within 120 minutes often with GPIIb/IIIa receptor antagonist IV then move to CCU. Anticoagulation during PCI (specialist advice) may be LMWH or UFH during PCI.
- Femoral route via the femoral artery to iliacs to abdominal aorta and then thoracic and arch and even into the left ventricle
- Radial artery is becoming a more popular route. Catheter passes along Brachial, subclavian and aortic arch down to the coronaries
- The catheter is then threaded into the Ostia of in turn right and left coronary arteries and radiocontrast dye given under x-ray imaging. Identifies and records coronary anatomy and any lesions. Dye can also be injected into the LV which will show LV function and aortic valve regurgitation
- The information provided can help the clinician decide the need for medical therapy alone or plus either PCI or CABG or Valve replacement if that is the pathology
- PCI centres should have individuals skilled in the procedure (>75 cases/year) In a high-volume centre (>200 cases/year)
- Intervention
- This can be done at the same time or planned for later
- A a fine wire can be passed into the artery and past the occlusive lesion via the coronary artery catheter and over this an angioplasty balloon can be threaded which could be inflated by an obstructive lesion. The problem was local damage, arterial dissection and subsequent restenosis and in some cases acute closure of the vessel (which could mean urgent bypass required). These made this a risky business. This was reduced by the use of stents
- Stents are mesh like tubes which splint the vessel open and reduce these complications. Stents are now indicated in almost all coronary interventions where there is identifiable disease-causing symptoms. Newer bare metal and drug eluting stents contain agents that reduce acute stent thrombosis and smooth vascular muscle growth. They require prolonged courses of antiplatelets.
- Additional agents (follow local guidance)
- With primary PCI : Aspirin Oral dose of 150-325 mg. Clopidogrel Oral loading dose of at least 300 mg, preferably 600 mg.
- GPIIb/IIIa inhibitors Abciximab: IV bolus of 0.25 mg/kg bolus followed by 0.125 mg/kg per min infusion (maximum 10 mg/min for 12 h)
- With fibrinolytic treatment: Aspirin Oral dose of 150-325 mg. Clopidogrel Loading dose of 300 mg if age <75 years; 75 mg if age>75.
- Without reperfusion therapy. Aspirin Oral dose of 150-325 mg and Clopidogrel Oral dose of 75 mg
Thrombolysis: first check indications and contraindications. Consider if PCI cannot be provided within 120 minutes of ECG.
- Streptokinase (Streptase) is indicated up to 12 hours after onset of symptoms. 1.5 million units over 30-60 min i.v. Cannot be used if given before due to the formation of neutralising antibodies. It is administered as an IV infusion over 1 hour. Associated with hypotension, infrequent allergic reactions and, rarely, anaphylaxis.
- Alteplase (recombinant human tissue plasminogen activator, rtPA) can be delivered in a standard or accelerated regimen. The accelerated regimen, which is much more commonly used, is indicated up to 6 hours after symptom onset and is delivered by an initial IV bolus injection, followed by two IV infusions, the first given over 30 minutes and the second over 60 minutes. The standard regimen is indicated between 6 and 12 hours after symptom onset and requires a bolus injection followed by five infusions over 3 hours.
- Tenecteplase is indicated up to 6 hours after symptom onset. Tenecteplase (TNK-tPA) Single i.v. bolus. 30 mg if < 60 kg, 35 mg if 60-70 kg, 40 mg if 70-80 kg, 45 mg if 80-90 kg and 50 mg if > 90 kg
- Absolute contraindications
- Haemorrhagic stroke or stroke of unknown origin at any time, Ischaemic stroke in preceding 6 months
- CNS trauma or neoplasms, Recent major trauma/surgery/head injury (within preceding 3 weeks)
- GI bleeding within the last month, Known bleeding disorder, Aortic dissection, non-compressible punctures (e.g. liver biopsy, lumbar puncture)
- Relative contraindications
- TIA in preceding 6 months, Oral anticoagulant therapy
- Pregnancy or within 1-week post-partum
- Refractory hypertension (systolic blood pressure >180 mmHg and/or diastolic blood pressure >110 mmHg)
- Advanced liver disease, Infective endocarditis
- Active peptic ulcer, Refractory resuscitation
Cardiac surgery
- There is still a role for Coronary artery bypass grafting. It may be a primary procedure for some or carried out after failed PCI and stenting or where the lesions are too high risk for PCI.
- The indications are those with
- LMS stenosis > 70%
- Proximal LAD stenois > 70%
- Triple vessel disease stenois > 70%
- Those with diabetes or Poor LV function are at higher risk but have most to gain. The operation is usually done on cardiopulmonary bypass through a median sternotomy.
- The plan is to bypass the existing stenotic lesions using either
- Left internal mammary grafted into the LAD beyond the stenosis. Arterial grafts have better long term patency.
- Reversed (they have valves) saphenous vein grafts from the legs to bypass coronary obstructive lesions.
- CABG patient is left with sternal wound and visible scars where veins stripped on lower legs if a reversed saphenous vein graft (SVG) was used.
Implantable Cardioverter Defibrillator
- VT/VF 24 hrs of more after admission
- EF < 35% 6-12 weeks after ACS