Makindo Medical Notes.com |
|
|---|---|
| Download all this content in the Apps now Android App and Apple iPhone/Pad App | |
| MEDICAL DISCLAIMER:The contents are under continuing development and improvements and despite all efforts may contain errors of omission or fact. This is not to be used for the assessment, diagnosis or management of patients. It should not be regarded as medical advice by healthcare workers or laypeople. It is for educational purposes only. Please adhere to your local protocols. Use the BNF for drug information. If you are unwell please seek urgent healthcare advice. If you do not accept this then please do not use the website. Makindo Ltd | |
CT Basics for Stroke
-
| About | Anaesthetics and Critical Care | Anatomy | Biochemistry | Cardiology | Clinical Cases | CompSci | Crib | Dermatology | Differentials | Drugs | ENT | Electrocardiogram | Embryology | Emergency Medicine | Endocrinology | Ethics | Foundation Doctors | Gastroenterology | General Information | General Practice | Genetics | Geriatric Medicine | Guidelines | Haematology | Hepatology | Immunology | Infectious Diseases | Infographic | Investigations | Lists | Microbiology | Miscellaneous | Nephrology | Neuroanatomy | Neurology | Nutrition | OSCE | Obstetrics Gynaecology | Oncology | Ophthalmology | Oral Medicine and Dentistry | Paediatrics | Palliative | Pathology | Pharmacology | Physiology | Procedures | Psychiatry | Radiology | Respiratory | Resuscitation | Rheumatology | Statistics and Research | Stroke | Surgery | Toxicology | Trauma and Orthopaedics | Twitter | Urology
Related Subjects: |Acute Stroke Assessment (ROSIER&NIHSS) |Atrial Fibrillation |Atrial Myxoma |Causes of Stroke |Ischaemic Stroke |Cancer and Stroke |Cardioembolic stroke |CT Basics for Stroke |Endocarditis and Stroke |Haemorrhagic Stroke |Stroke Thrombolysis |Hyperacute Stroke Care
Introduction
- Stroke medicine did not really develop into a proper speciality until the arrival of the CT scanner and the increasing access to early imaging that could tell us if there was a stroke and if that stroke was likely to be ischaemic or haemorrhagic. A simple non-contrast CT head can be done on anyone (unlike MRI) if they are claustrophobic (most scanners are fairly open), if they are unwell (they take less than a minute and they can be monitored throughout), if they have metal fragments (there is no magnet). CT is much faster than MRI with shorter image acquisition times. The only catch is that changes on CT for an early ischaemic stroke can be subtle or it can appear normal so initially the rationale for CT is that a clinical stroke syndrome with no haemorrhage is assumed to be an ischaemic event if within the first 6 hours and this is good enough for thrombolysis.
- CT imaging forms the basis of stroke care as it can rapidly differentiate between Ischaemic and Haemorrhagic stroke and some stroke mimics. All clinicians need to develop competencies in reading CT scans and identifying what is normal and what is not. The best way to learn is to look at all the scans which you request, to attend a weekly neuroradiology meeting and to spend time learning the cross-sectional anatomy and vascular supply. Looking at scans is part of good stroke practice and the correlation and sometimes lack of correlation between clinical findings and imaging can be vitally important. Looking at imaging isn't just for medical staff but something that should be of interest to all involved in stroke care. In some centres specialist nurses and therapists attend the neuroradiology meetings and this helps to educate all.
- It wasn't always this way. I inherited a copy of Brain's clinical neurology from the 1970s and there isn't a single cross-sectional image in the whole book as it didn't exist. Prior to CT there was no reliable way to diagnosing haemorrhage versus ischaemia other than at post mortem. Various clinical scoring systems were developed but were unreliable. A calcified pineal good give some idea of where the midline was and tell if it had shifted but it is hard to think that was very useful and I suspect craniectomies were done for suspected haemorrhage which never were. It was really a forlorn attempt at gathering information. No wonder the feeling of diagnostic futility led to a very negative view of stroke. How times change. It's still a surprise that even with the amazing advances in imaging that we still have to deal with diagnostic uncertainties and the answers are not always clear.
History of CT Imaging
- The first CT scanner was developed in 1972 by Sir Godfrey Hounsfield who was a researcher at EMI. It's a fascinating fact that it was the wealth derived by record sales from the Beatles who were signed to EMI that funded early CT research. Hounsfield went on to win a Nobel prize. It was Hounsfield who came up with the idea that one could determine what was inside a box by taking X-ray readings at all angles around the object. He then built a computer that could take input from X-rays at various angles to create an image of the object in "slices".
- Applied medically this became computed tomography. Hounsfield built a prototype head scanner and tested it first on a preserved human brain, then on a fresh cow brain from a butcher shop, and later on himself. On 1st October 1971, CT scanning was introduced into medical practice with a successful scan on a cerebral cyst patient at Atkinson Morley Hospital in Wimbledon, London, United Kingdom.
- It wasn't until the mid to late 80's that CT was available initially in teaching hospitals for assessing stroke patients. Prior to this, there was no way to discern ischaemic and haemorrhagic strokes ante-mortem. The CT scanner consists of an X-ray tube and on the opposite side of the cylinder where the patient lies is a set of x-ray detectors. Through a process of data acquisition, the X-ray tube and detectors rotate 360 degrees around the patient in the x and y plane and acquire a vast amount of imaging information which then undergoes image reconstruction. The tube also moves in the z-axis so building up a 3 d image.
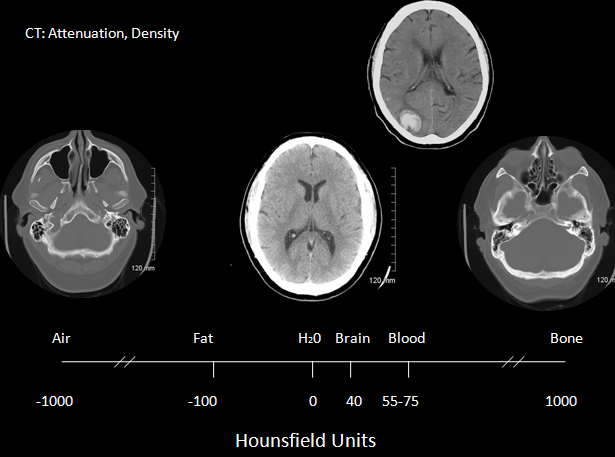
- Spiral CT was developed in the early 1990s and improves scan speed and flexibility. The x-ray tube and detectors rotate continuously about the patient while the scan table advances the patient continuously through the gantry. Between the x-ray tube and the detectors, there is a loss of attenuation as it travels through structures and this is known as the attenuation coefficient which reflects the degree to which the x-ray intensity is reduced by the material. These values are scaled to give values known as Hounsfield units seen in the table below. The overall appearance can be altered by varying Window level and window width. Different windows can be used to look at different structures as shown below. Helical scans mean that there is a continuous movement of the patient through the gantry whilst imaging. Multislice scanners mean that anything from 16-64 slices may be acquired at one time. For CT head slice thickness, is typically 5 mm for a standard head CT and between 0.625-1.25 mm for CTA. Although there is a wide number of Hounsfield numbers the human eye can only differentiate less than 100 different levels of grey.
Different Hounsfield units
| Medium | Hounsfield Units | Appearance |
|---|---|---|
| Air | -1000 | Black |
| Fat | -80 to -100 | Black |
| Water | 0 | Black |
| CSF | +5 | Black |
| White matter | +30 | Dark Grey |
| Grey matter | +40 | Light Grey |
| Acute haemorrhage | +70 | White |
| Bone | +400 to +3000 | Bright White |
Radiation Exposure
- CT involves exposure to ionising radiation and so care must always be taken in its use. In the UK access to scanning is guided by IRMER guidelines and only trained professionals can request scans which includes appropriately trained doctors, specialist nurses and radiographers and radiologists.
- In many trusts have protocols (See indications for urgent CT scan)and agreements that allow specialist stroke nurses to arrange urgent Head CT scans without medical input. This is a vital time-saving step in those who need acute therapies and experience tend to show that this works well. CT scans should only be done when there is a clear clinical need and the result will help to direct therapies or provide useful information that can alter management.
- A typical head CT involves exposure to 2.1 milli-Sieverts (mSv) but can often be more. For comparison, 10 millisieverts (mSv) of radiation is the rough equivalent of 200 chest X-rays. An increased risk of cancer has been identified among long-term survivors of the Hiroshima and Nagasaki atomic bombs who received exposures of 10-100 milliSieverts so care must be taken. Obviously denser structures need greater doses of radiation. Risk can be measured here.
| Scan | Dose |
|---|---|
| Natural Background | 3.1 mSv/year |
| Domestic pilots | 2.2 mSv/year |
| Average US Exposure | 6.2 mSv/year |
| CXR (AL and lateral) | 0.10 mSv/year |
| Chest CT | 7.0 mSv/year |
| Chest Abdomen Pelvis CT | 21.0 mSv/year |
| Brain CT (standard) | 2.0 mSv/year |
| CTA/CTP Head | 16.4 mSv/year |
Contraindications
Clinically there are no real contraindications for CT if clinically indicated. There are no concerns about pacemakers or defibrillators or metal clips or recent surgery. It is probably unwise if the patient is moribund and too unwell for any intervention and better served by palliation but that's a specialist call. Scans are incredibly quick nowadays and patients can be closely monitored. The only real difficulty is with agitated or confused patients in whom scan quality will be degraded with movement artefact. A doctor can be at the side of the patient during a CT with an appropriate lead apron or behind a screen for protection if needed. CT does not prevent monitoring equipment of infusions or drips. It may be occasionally necessary to intubated and ventilate a patient prior to scanning.
Non contrast CT scan in Ischaemic stroke
Non-contrast CT scan is the standard imaging modality for hyperacute stroke care. It is fast, cheap, accessible, and very sensitive for haemorrhage and there is no problem with pacemakers or monitoring equipment. Claustrophobic or monitored patients can be scanned relatively easy. Done early many scans will be normal despite significant clinical findings. Stroke is primarily a clinical diagnosis and not a radiological diagnosis.
Indications for urgent CT scan
| Clinical Indications for urgent CT i.e. within 1 hour of arrival at hospital |
|---|
|
CT and Windowing
This involves a mechanism by which one can select for different Hounsfield numbers. Used well it can help increase the contrast between various structures. For example, a window of 2000 will show most CT numbers. A wide window (W) 400-2000 HU is useful for showing low and higher density tissues. A narrow window 50-350 HU is better at showing soft tissue. Window Level (L) is the midpoint of the CT range. The brain is W80:L40, Stroke is W8:L32 or W40:L40.
| Indication | Parameters |
|---|---|
| Brain window to best show white/grey matter differentiation | W=80 L=40 |
| Bone windows for bone pathology | W=3500 L=700 |
| Subdural windows for small or isodense subdurals | W=250 L=70 |
What may be missed on a CT Scan
CT is incredibly useful but not infallible and its limitations should be respected. A normal CT scan is entirely compatible with a large ischaemic stroke when within 6 hours of onset. There may be some subtle early changes. CT is also very poor at picking up changes in tissue density in bony spaces such as temporal bones and posterior fossa due to what is called beam hardening as the x-ray beam is distorted by the dense bone traversed. Metallic objects such as aneurysm clips or piercings that weren't removed can cause a radiating streak pattern. Partial volume artefacts can cause streaks or bands of alternating dark and light stripes and beam hardening also affect the posterior fossa. CT scanning cannot differentiate between hypodensity due to infarction or haemorrhage after 1-2 weeks and MRI with GRE or T2* must be used. Subacute ischaemic stroke after several days can show haemorrhage and irregular patterns of density and haemorrhagic changes which can resemble tumour s. Follow up interval scanning will be needed.
| Caution : What may be missed on a CT scan |
|---|
|
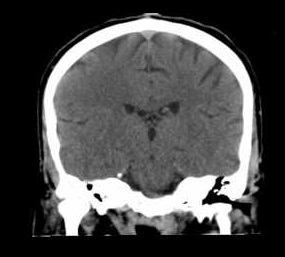
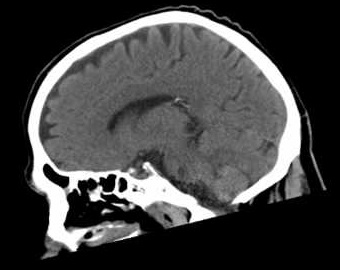
Make sure you understand the terms axial, sagittal and coronal. Axial is simple horizontal slices from above down. Sagittal is in the same plane as cutting the brain in the midline or parallel to this (parasagittal). The falx cerebri that separates the brain hemispheres lies in the sagittal plane. Coronal is like a tiara or 'corona'. It is vital to have a good inner representation of the cerebral vessels as they enter the skull and join the circle of Willis and the circle of Willis as well and the position of the vessels. A few simple points will help greatly. The circle of Willis (COW) is at the level of the midbrain. Find the midbrain and then look for the vessels. This is a good place to start looking for the hyperdense MCA as the MCA leaves the COW laterally within the Sylvian fissure.
| Axial | Coronal | Sagittal |
|---|---|---|
 | 
|  |
Looking at Imaging
Starting with imaging. It is important to take your time and go through each slice from top to bottom in every case. Don't be distracted by the most obvious "big" finding and make sure you take time to ensure that you don't miss things. This is even more important in thrombolysis cases where the main concern is "is there any blood" and great care must be taken in what is a time-pressured environment. In that situation, I look at the scan whilst it is being done in the CT and then as soon as the patient is out and before we give open the Alteplase I will go off to a monitor away from the team and distractions and quickly go through all the slices without interruption at least twice. As I have become more experienced and seen more and more cases I think this level of care is important. It's one of the reasons why I don't rush to give Alteplase in the CT scanner as the control room is not the best place to look at a scan with diagnostic quality. I feel that several minutes quickly reviewing the scan in a controlled way is important especially in patients where things may just not seem clinically right. In most cases, we do not get a radiology review before lysis. I will actively look for any suggestion of a thin layer of subdural blood or any hyperdensity that might reflect acute bleeding. Sometimes it is difficult if there is asymmetrical basal ganglia calcification that can mimic blood or it may actually be blood. I will take particular care to look for any subarachnoid blood within the ventricles and cisterns as well as convexity blood in the sulci. I have seen excellent colleagues caught out with very subtle basal ganglia blood that looked very much like calcification even when shared with the neuroradiologist and also subtle sulcal convexity blood probably due to cerebral amyloid. One possible clue is that often the NIHSS if the neurology is due to very subtle haemorrhage is usually in that low threshold to treatment range. The rest of the time scans can be looked at with time. It is very important whatever stage you are at the look at every scan. It may not mean much at the start but you are building up your own visual memory bank of imaging with which to compare every new scan and it quickly trains your visual skills.
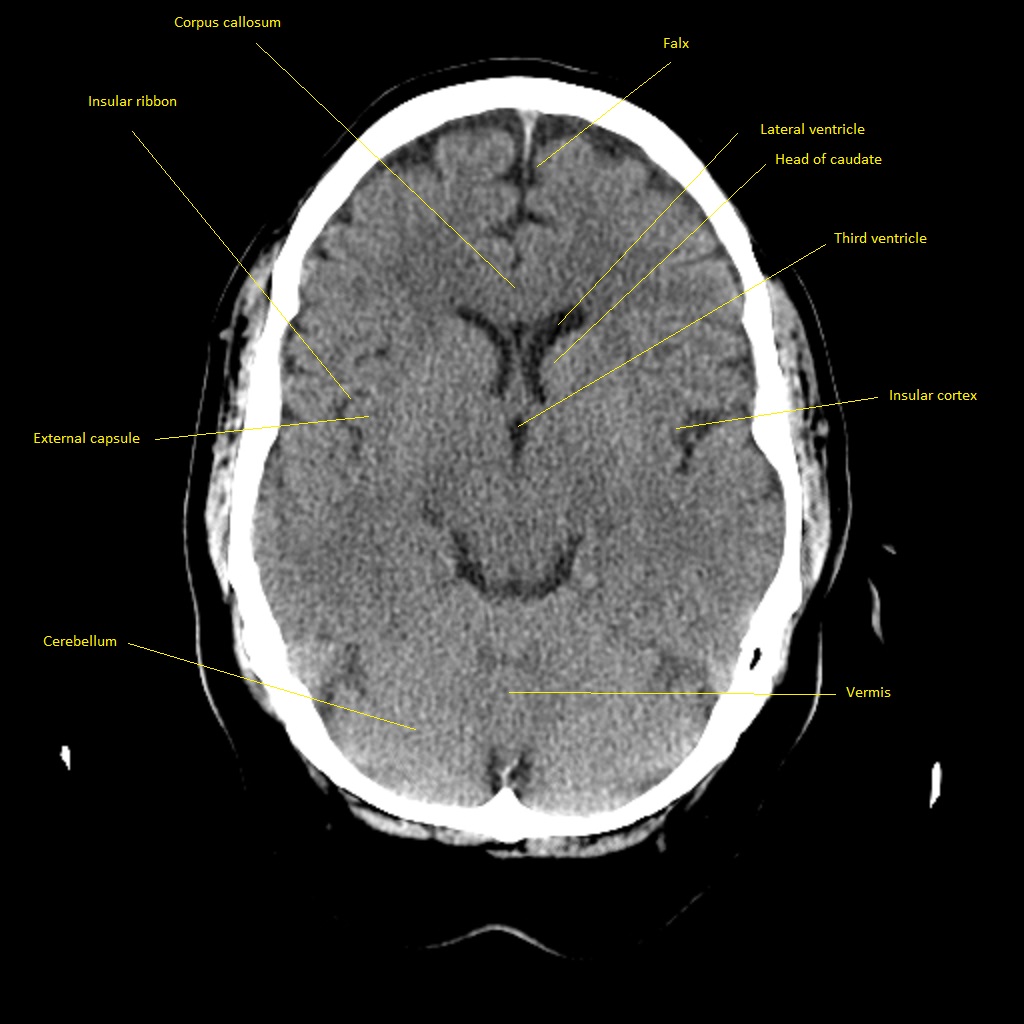
Normal Cross sectional CT anatomy
Top down Axial Imaging
Image below:The top image two slices here are useful for just ensuring that there is no subdural blood or any other abnormality. It is on the top few slices that we may see a subtle anterior cerebral artery infarct that can have caused contralateral leg weakness and these slices must be looked at very carefully. It is important to recognise calcification of the choroid plexus which is within the ventricles and produces CSF. It is possible to get a focal haemorrhage up at this level. Each slice needs careful review.
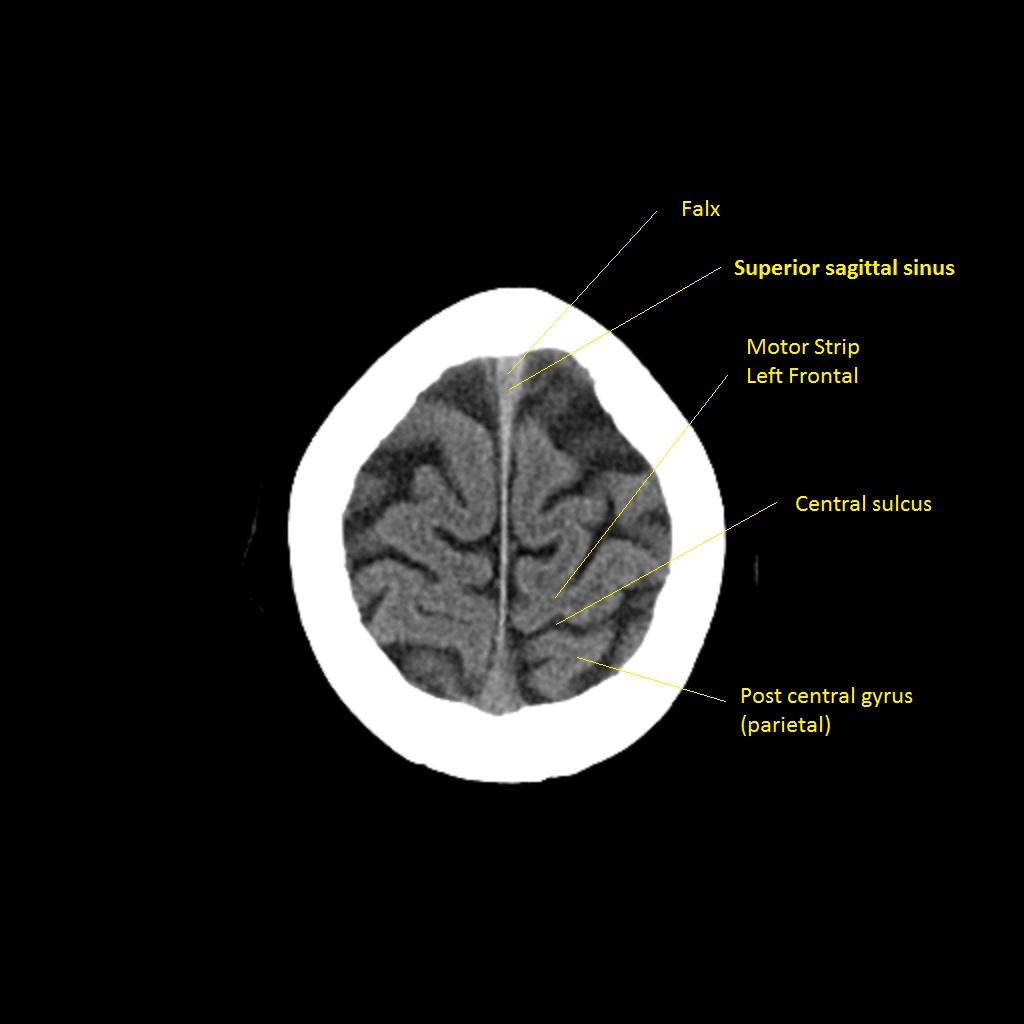
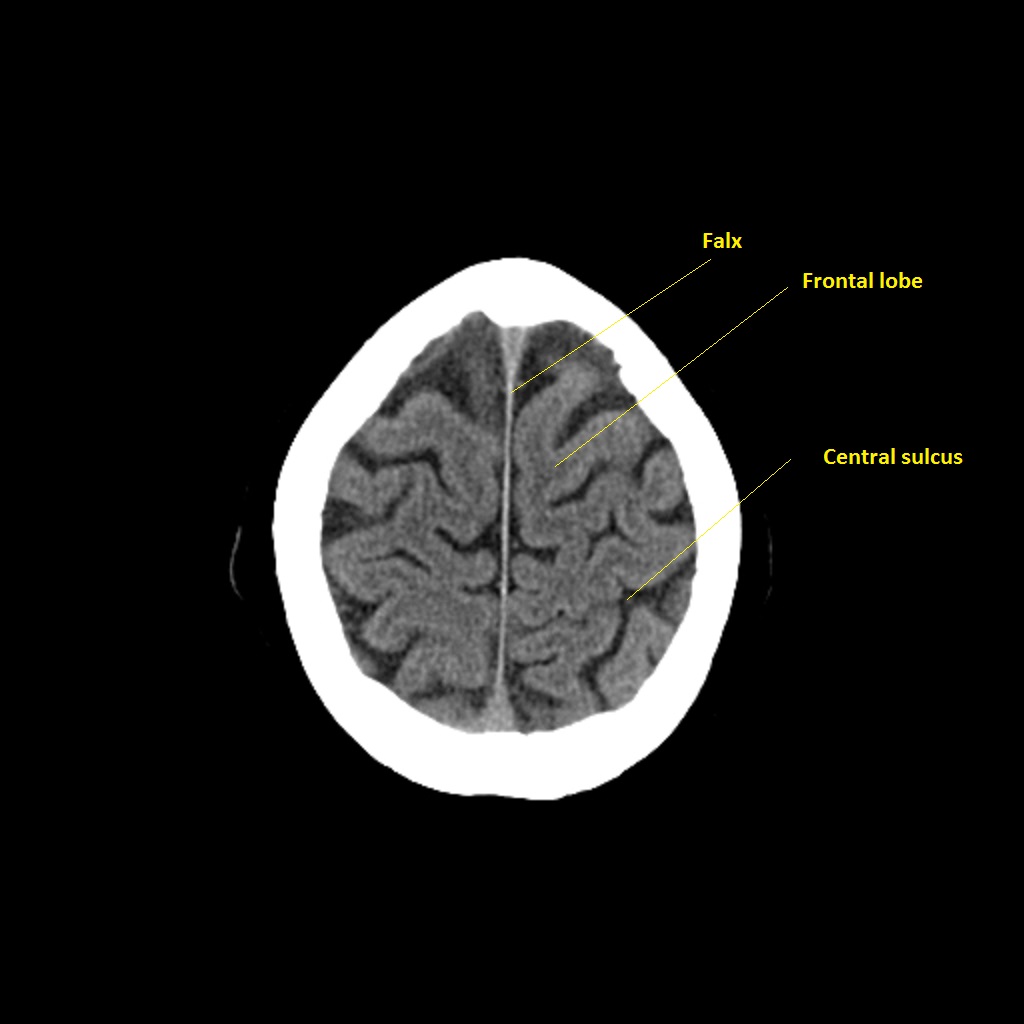
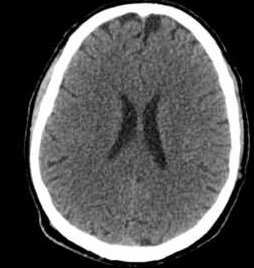
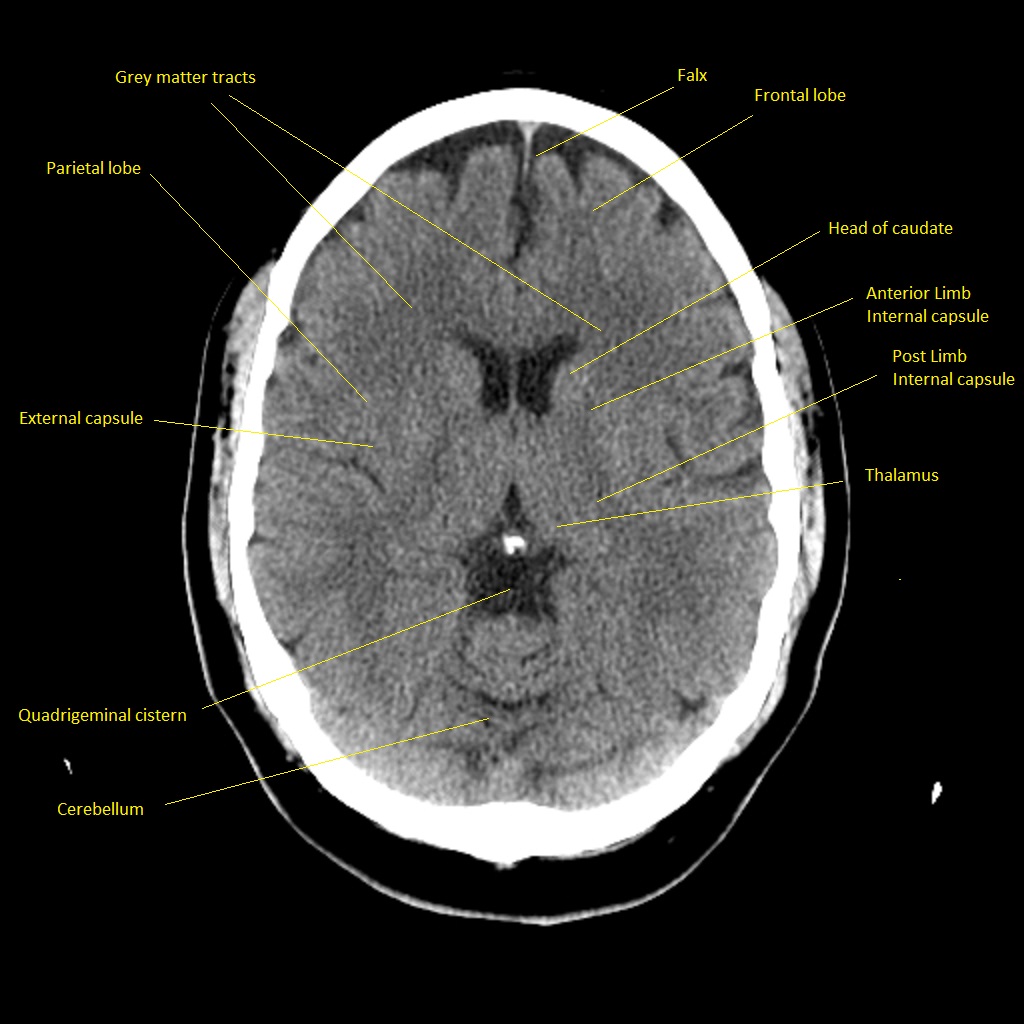
Image below:A good view to look for any evidence of parenchymal abnormality in the cerebral hemispheres. Here we have brain supplied by ACA, MCA and PCA. Look for any asymmetry and look closely for any space between the parenchyma and the inner skull that could be subdural. Appreciate the contrast between the outer grey matter and the more central darker white matter.
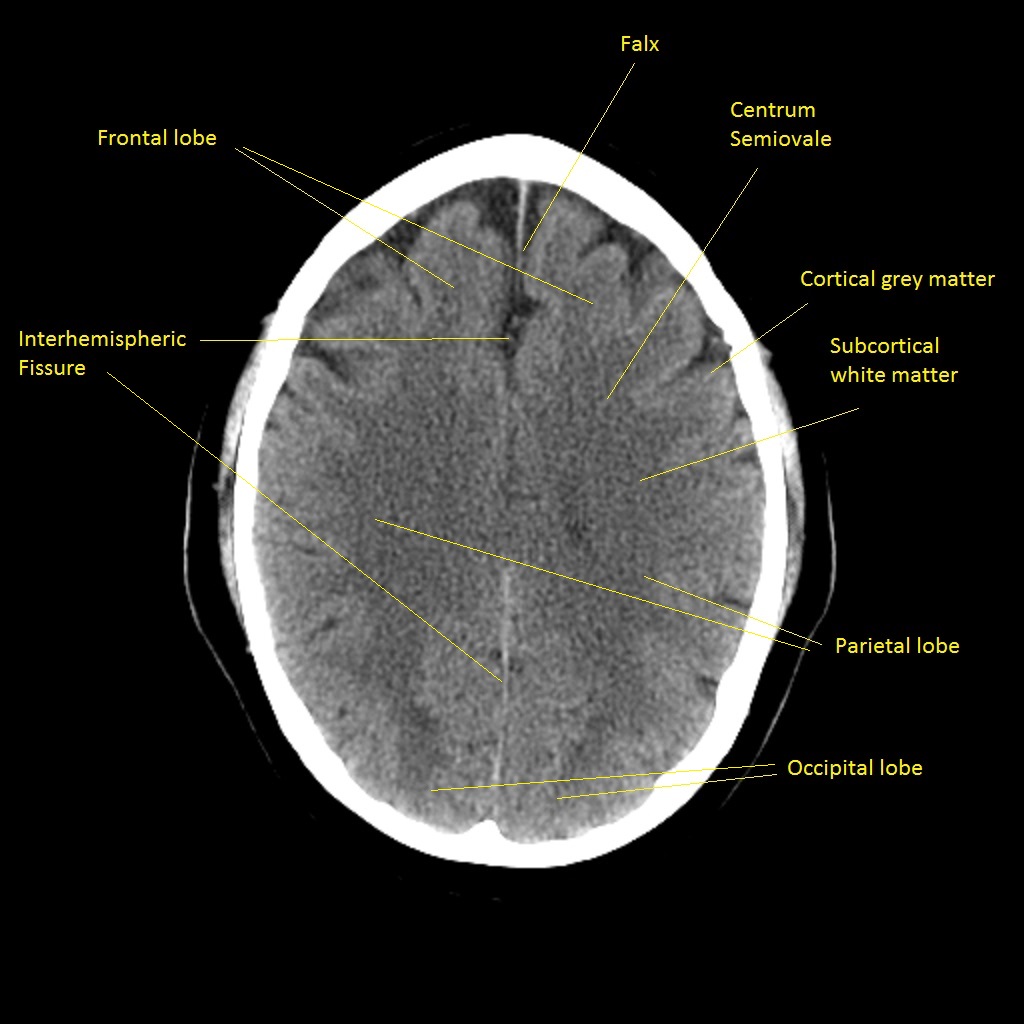
Image below:A good view to look for any evidence of parenchymal abnormality in the cerebral hemispheres. You can also see the frontal and temporal horns of the lateral ventricle and the slit-like third ventricle. Any enlargement of these particularly the temporal horns can suggest hydrocephalus.
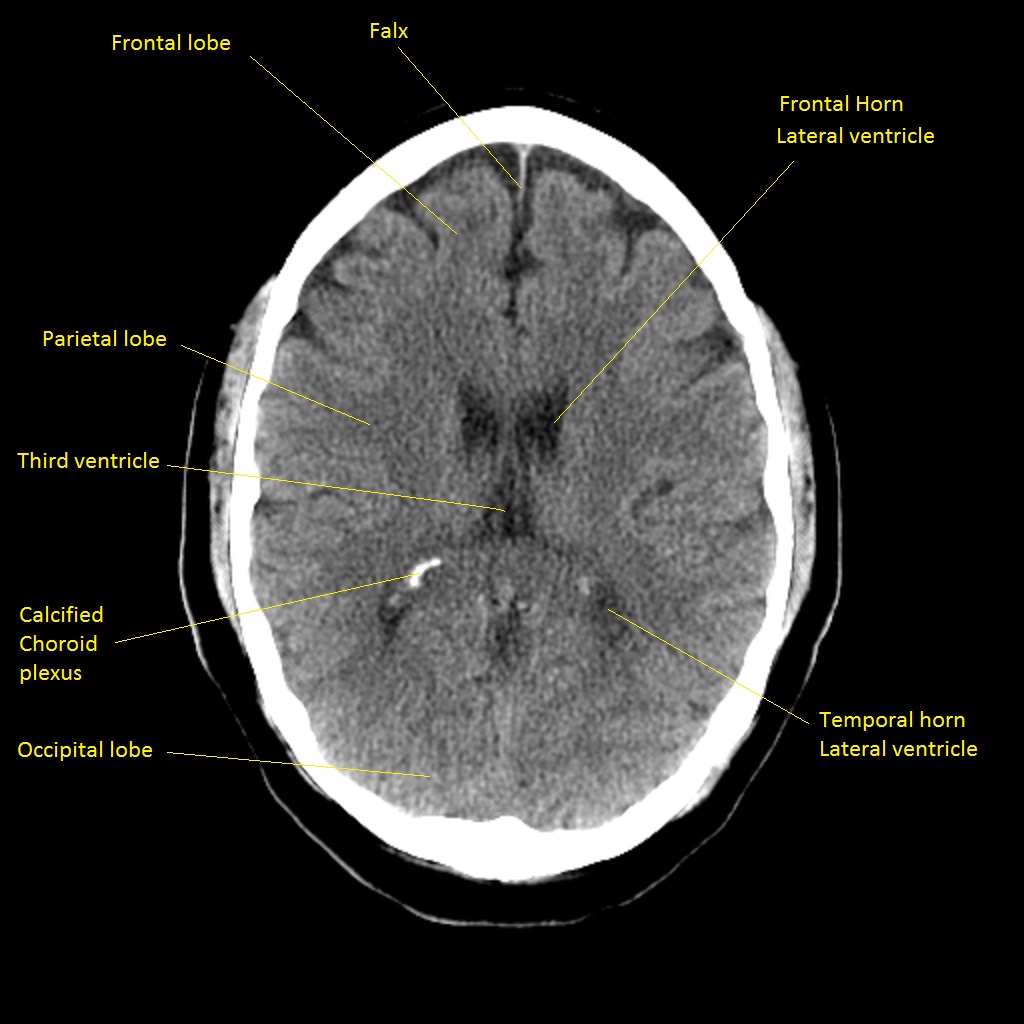
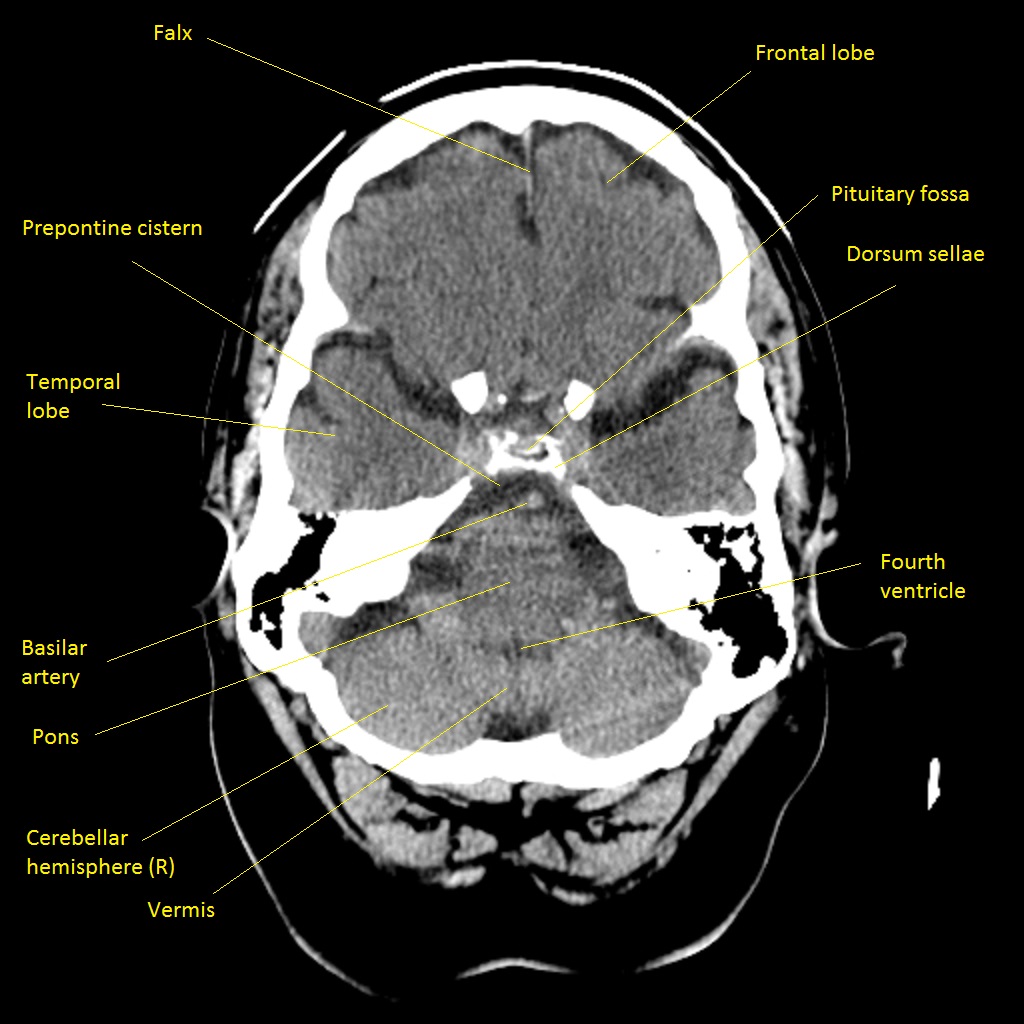
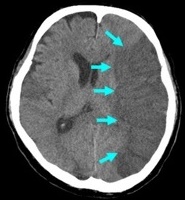
Image below:This is the level going through the Midbrain. Identify the V shape of the midbrain. This is formed by the cerebral peduncle which carries the descending motor fibres in the front of the "V". This is a good position or a slice above or below to see the branches of the circle of Willis and this is often the level at which one can see clot "the hyperdense artery sign" within the MCA or even PCA. You can also see the frontal and temporal horns of the lateral ventricle and the slit-like third ventricle. Any enlargement of these particularly the temporal horns can suggest hydrocephalus.
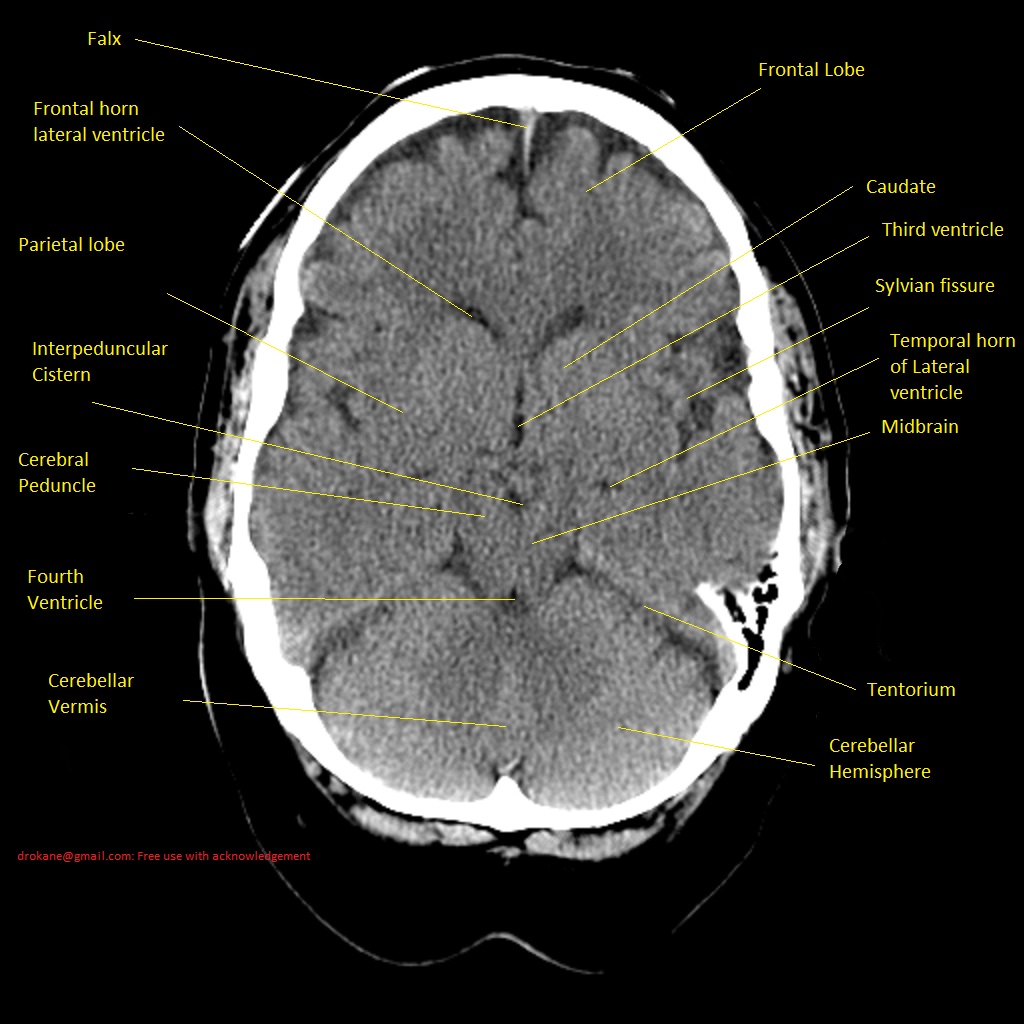
Image below:This is the level going through the Upper Pons. As you can see the pons is a slightly rounded structure with the cerebellum attached posteriorly separated by the fourth ventricle. This a common area to contain blood in those who have had bleeding into the ventricular system.
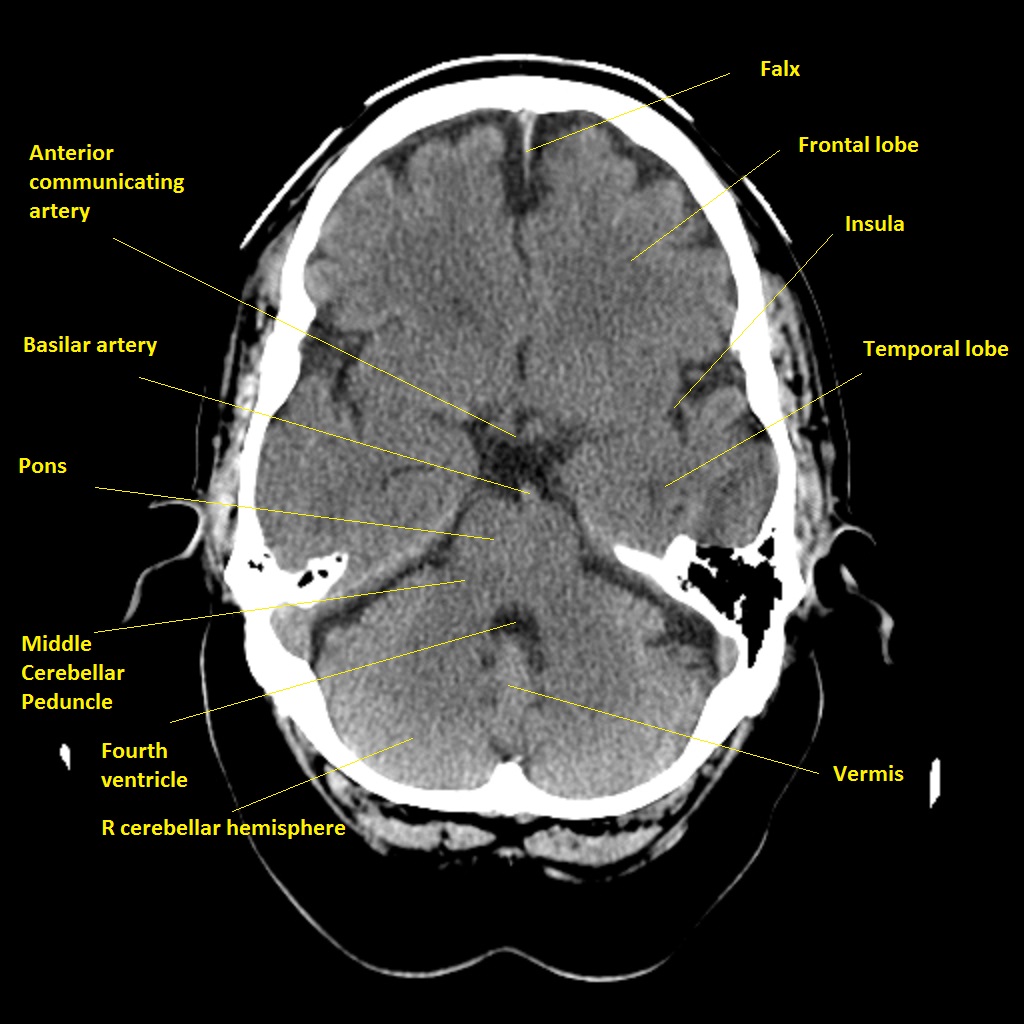
This is the level going through the lower Pons
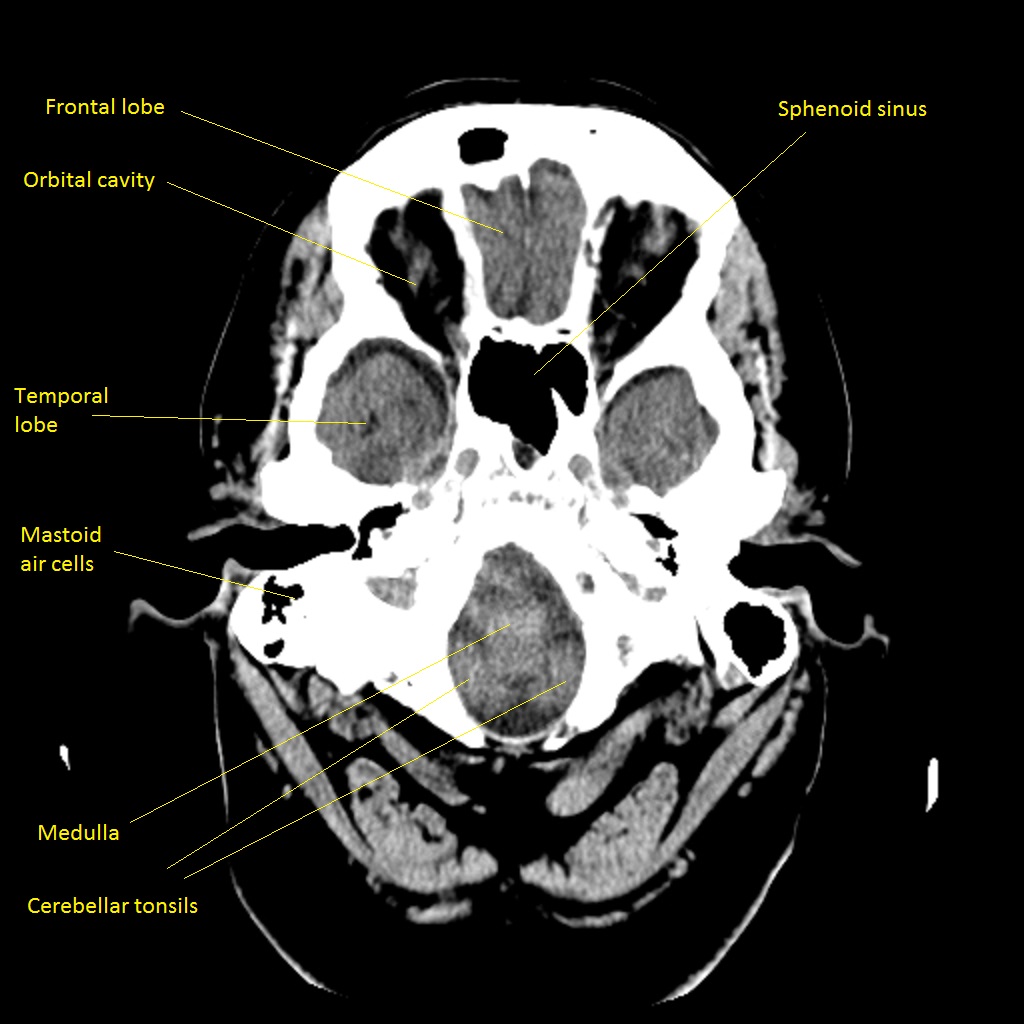
This is the level going through the medulla
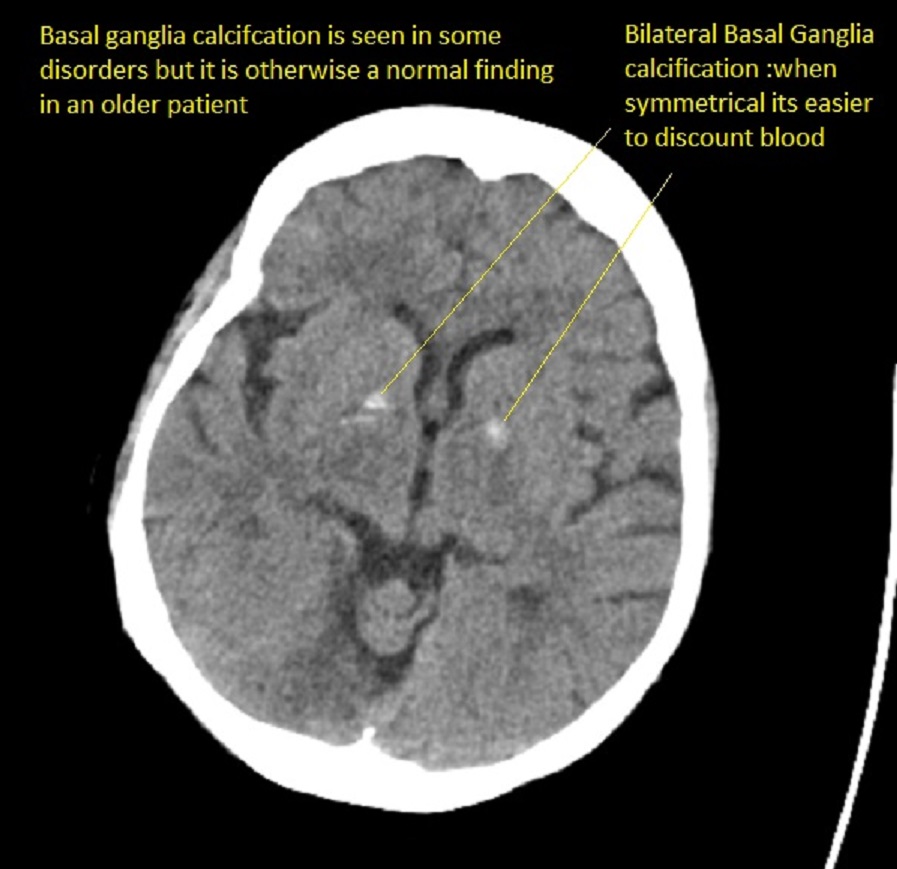
Basal Ganglia calcification
Some degree of basal ganglia calcification is normally seen and the main issue is to differentiate it from blood. There are extreme variants and the so-called Fahr syndrome. Normal calcification is seen in middle age and beyond. Unless extreme it is rarely associated with any problems.
Introduction
It is important to develop your ability to study imaging and correlate it with brain structure and function. There is a standard anatomical vocabulary with terms such as axial, sagittal and coronal which are commonly used in both CT and MR to describe different cross-sectional images. Modern-day imaging actually allows the brain to be imaged and reconstructed in any plane but these are the standard and familiar views.
Look at as much brain imaging as possible, the ones that you request and more. The key is to see a wide variety of normality and to build up some pattern matching skills and experience in identifying important structures and lesions. You will have an advantage over the radiologist who has only the clinical details on the card whereas you have the patient.
CT Interpretation
Definitive distinctive changes may not occur until 6-8 hours. In the meantime, more subtle signs are seen. At about 6 hours and sometimes earlier there may be loss of grey-white matter differentiation - seen at the cortical surface due to localised changes such as cytotoxic oedema within the grey matter which has a higher metabolic requirement and so becomes oedematous quicker. These signs are subtle and can be missed by even the most experienced
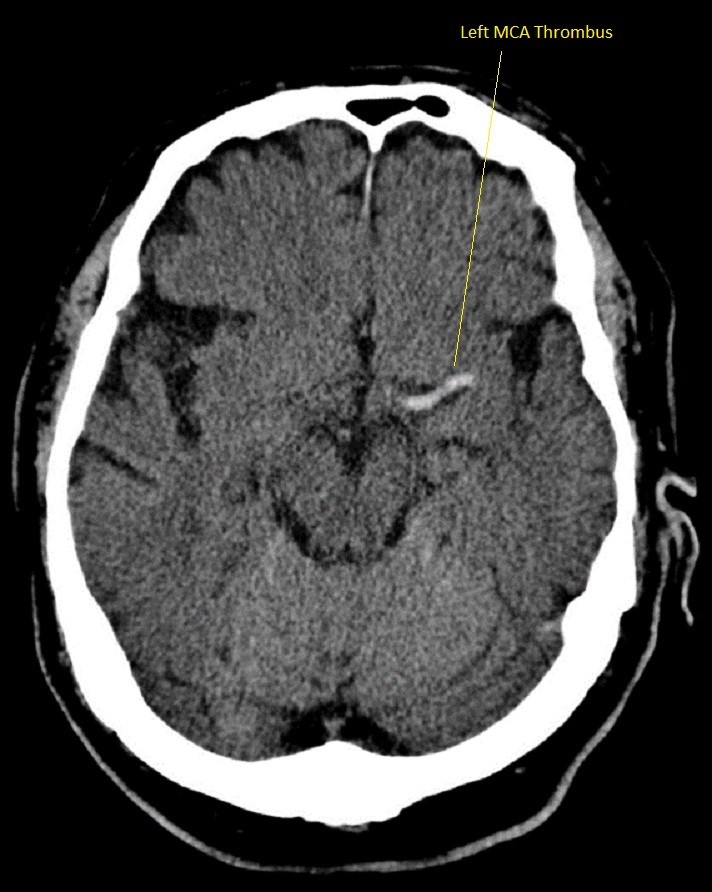
Left MCA hyperdense artery
This can be the earliest sign of a large vessel stroke is accompanied by a corresponding Left MCA stroke syndrome. There are no obvious tissue changes and the patient is within the window and NIHSS is raised and no contraindications should be considered for thrombolysis/thrombectomy if safe. Occasionally due to good collaterals, there may be minimal symptoms and in others, they can be profound. A dense artery may just be calcium in the vessel wall and scans must be interpreted within the clinical context.
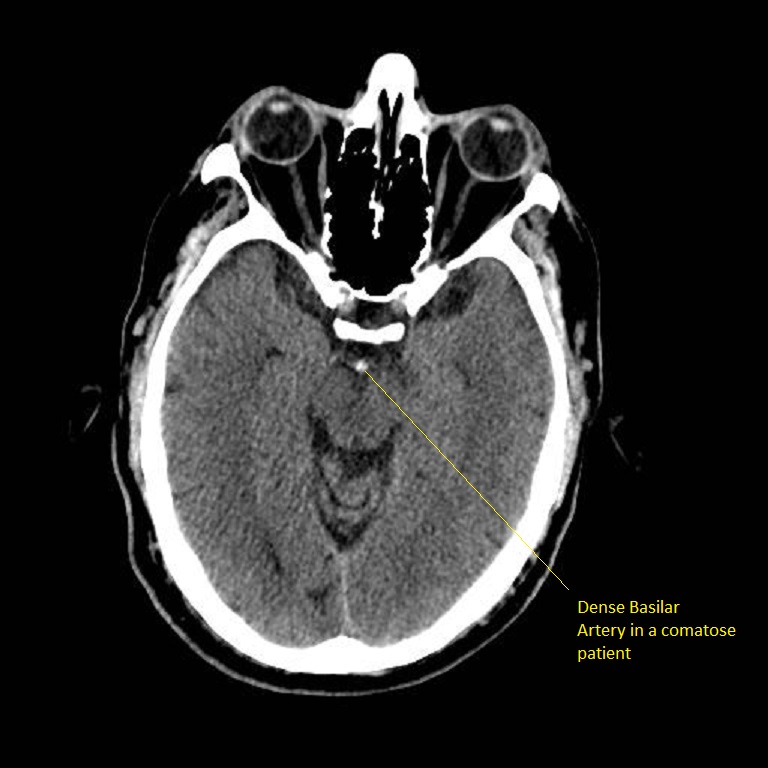
Dense Basilar Artery
The patient was comatose and sustained massive damage to the posterior circulation. This is an important sign in a deteriorating and comatose and quadriplegic patient needing consideration for thrombectomy. There are no parenchymal changes seen yet.
Early signs: less than 6 hrs of Acute Ischaemic Stroke
- May be entirely normal initially
- Cortical Sulcal effacement - suggests some increased oedema
- Loss of Grey/White differentiation in the basal ganglia
- Loss of insular ribbon sign is similar to the loss of grey-white differentiation with localised cytotoxic oedema. Vascular supply here is more vulnerable due to poor collateralisation and so this may show first.
- Obscuration of the Sylvian fissure: Similar to insular ribbon sign
- Hypoattenuation seen on CT is highly specific for irreversible ischaemic brain damage and infarction if it is detected within the first 6 hours.
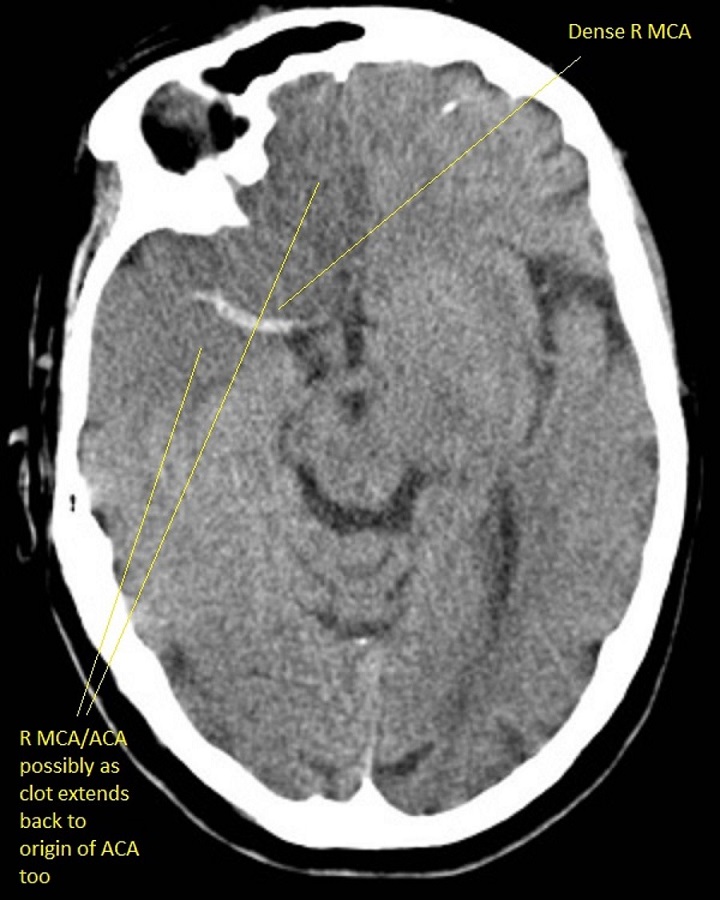
- Hyperdense MCA sign or more distal MCA "dot sign" it may be normal is a sign of clot (thrombotic or embolic) (not a contraindication to lysis) but shows the extent of possible infarct which depends also on collateral flow.
- Obscuration of the lentiform nucleus (loss of the normal attenuation difference of the globus pallidus and/or putamen with respect to contiguous white matter structures
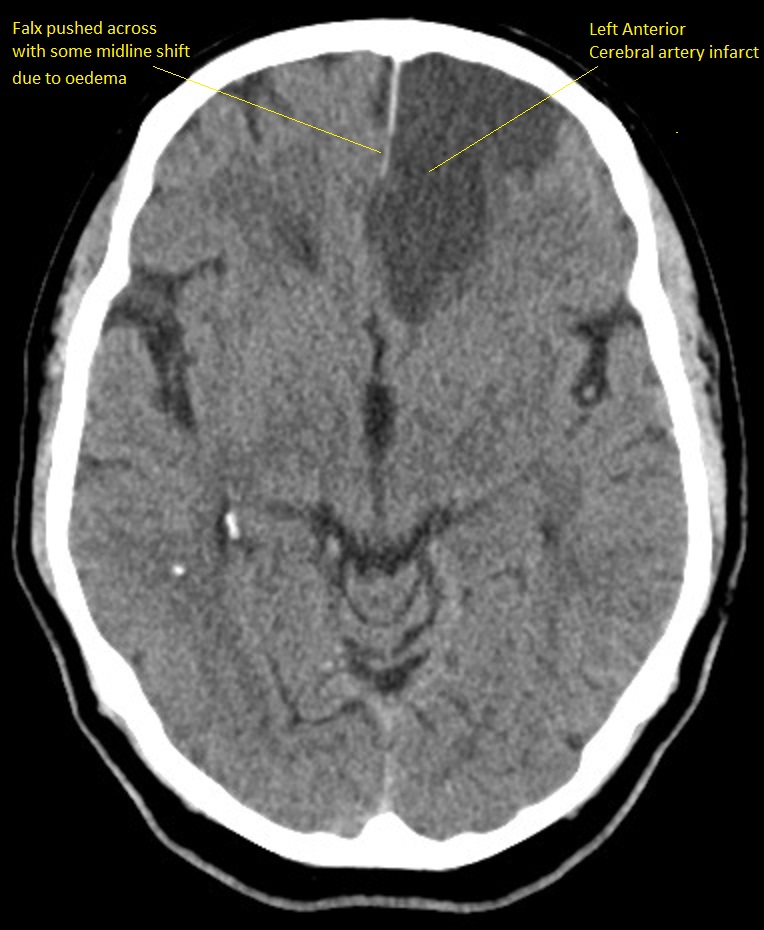
Developed Anterior Cerebral Artery Infarct
This shows an evolved subacute infarct as the edges are still indistinct and so there is ongoing liquefactive necrosis. This is about Day 2-4 or beyond. There is some mild midline shift due to some localised oedema.
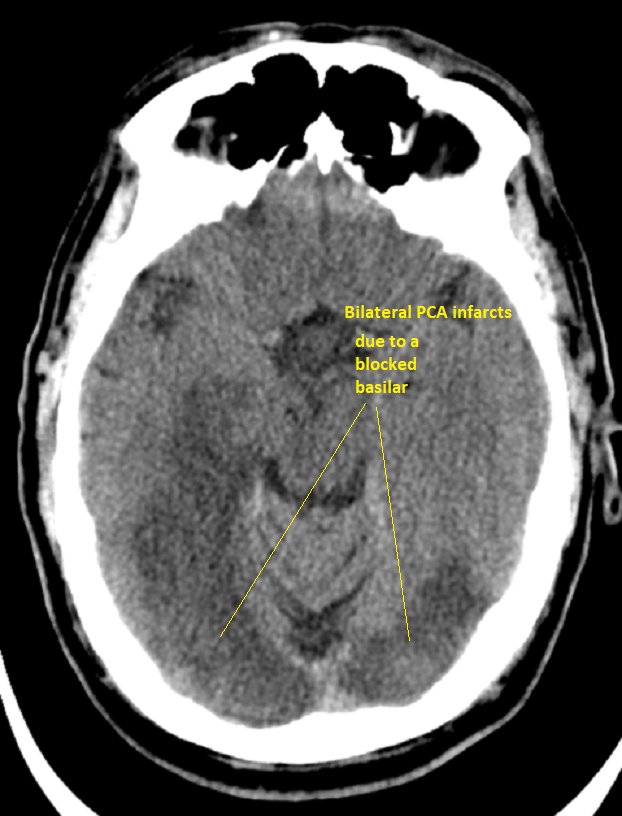
Bilateral PCA infarcts due to Basilar occlusion seen above
Infarction involves both occipital lobes. The patient who survived is blind.
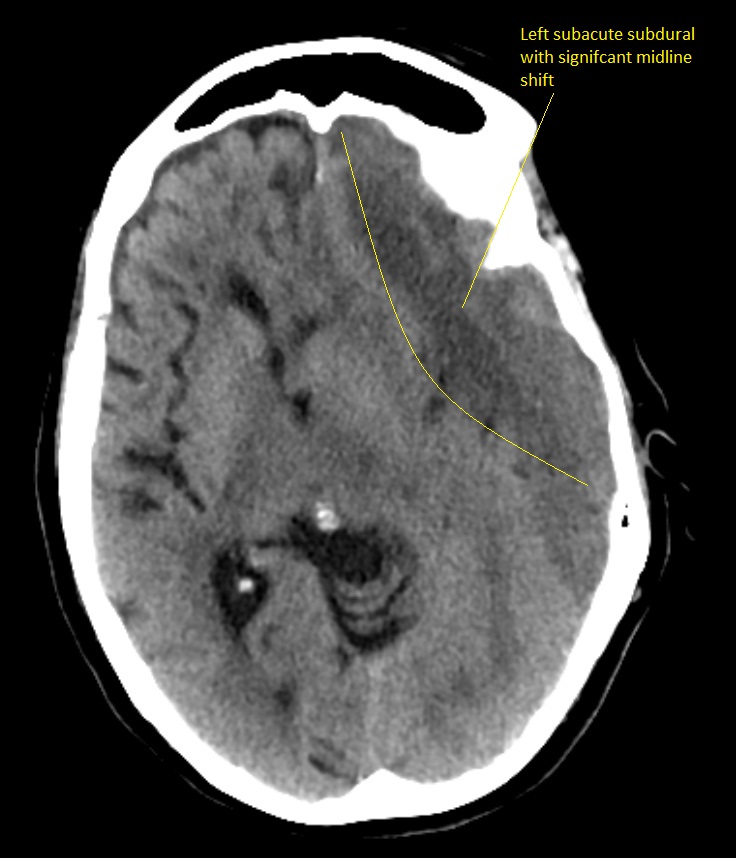
Large left Subdural Haematoma
There is no bright white fresh blood so this is a subacute bleed and it can be surprising how well these are tolerated. The midline is shifted. This is not stroke. It needs urgent discussion with neurosurgeons. Any anticoagulants or antithrombotic therapy must be stopped. The decision on whether to operate will depend as well on the clinical state of the patient.
| Later signs (6-24 hrs) of Acute Ischaemic Stroke | |
|---|---|
|
|
| Late signs ( > 24 hrs) of Acute Ischaemic Stroke | |
|---|---|
|

|
Non-contrast CT false negatives (there is a stroke) usually in infarcts when done early or in those who present 7-10 days after stroke and there is a visible hypodensity but no blood and so aetiology of perhaps a small bleed may be missed. In these cases, a gradient echo will show haemosiderin deposition around the margins suggesting haemorrhage as he cause.
NCCT false positives are seen particular in older hypertensive patients where Lacunar infarcts are common and most often asymptomatic but appear on scans done for a myriad of reasons so unless there is corresponding new neurology do not diagnose acute stroke but do treat for "stroke disease".
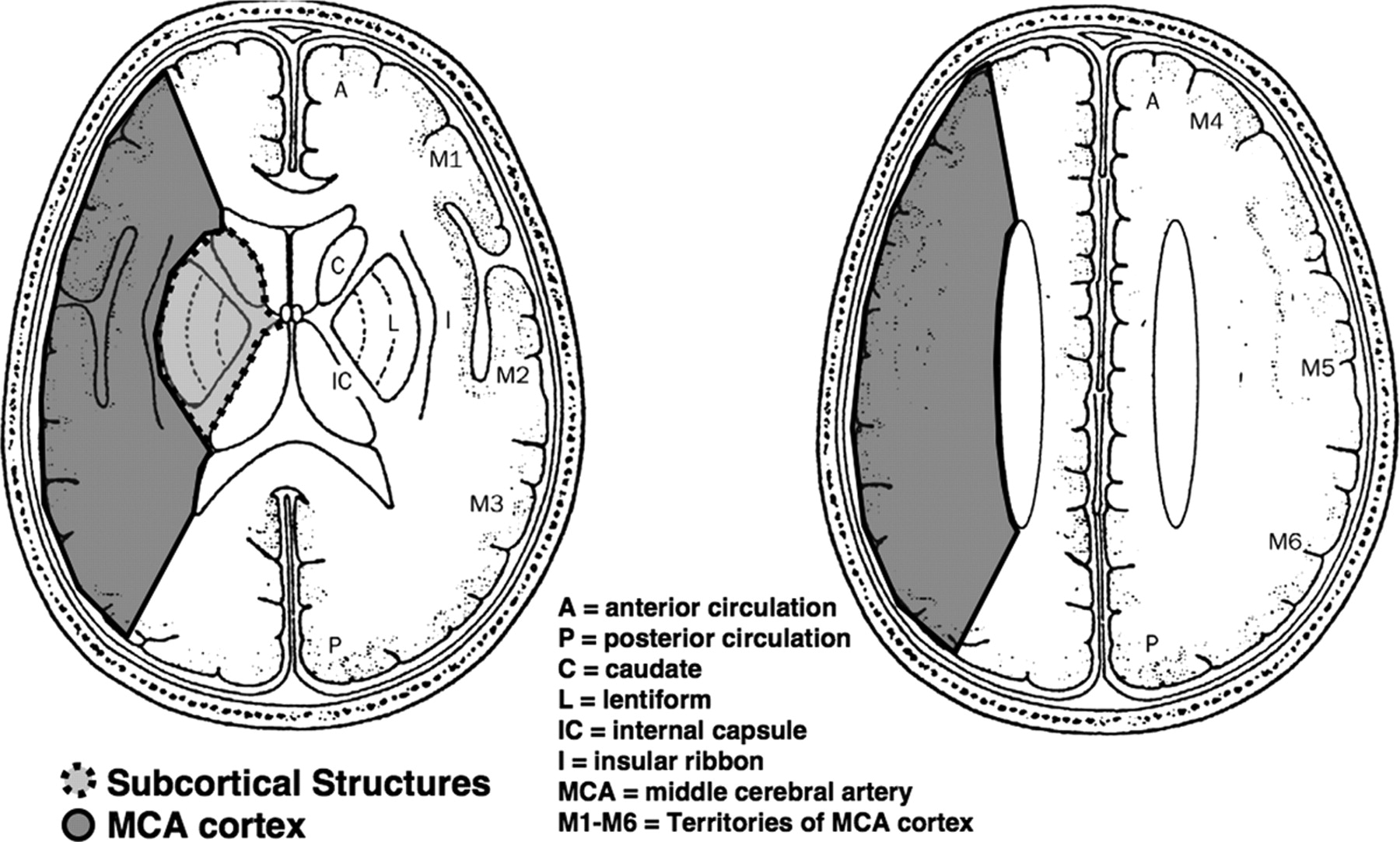
ASPECTS
The Alberta Stroke Program Early (non-contrast) CT score (ASPECT) is a scoring system used to assess the extent of early ischaemic changes in the middle cerebral artery territory on non-contrast computed tomography. The clinician/radiologist studies the appearance at two different axial slices corresponding with two different anatomical levels and subtracts 1 from the total maximum of 10 for each area affected. A score of 0 suggests extensive MCA infarction and correlates inversely with NIHSS. A score of 10 is normal. An ASPECTS score less than or equal to 7 predicts a worse functional outcome at 3 months as well as symptomatic haemorrhage. Online training and more information is available from link
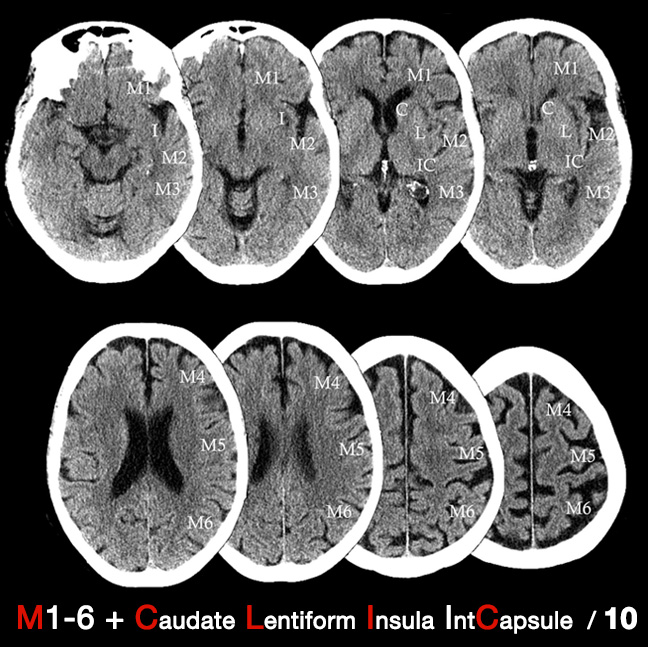
| Basically the higher the ASPECTs score the better the prognosis. High scores such as 10 are normal and low scores < 5 suggests evolved ischaemic changes. |
| A normal CT scan has an ASPECTS of 10 points. One point is subtracted for ischaemic changes in each region of the MCA territory. | |
|---|---|
| Lentiform nucleus level / Subcortical Structures | |
| M1 Anterior MCA cortex (Frontal operculum) | -1 |
| M2 MCA cortex lateral to the insular ribbon (Anterior temporal lobe) | -1 |
| M3 Posterior MCA cortex (Posterior temporal lobe) | -1 |
| Lentiform (L) | -1 |
| Caudate nucleus (C) | -1 |
| Internal capsule any part (IC) | -1 |
| Insular ribbon/cortex (I) | -1 |
| Centrum semiovale level | |
| M4 (Anterior)superior to M1 | -1 |
| M5 (Lateral)superior to M2 | -1 |
| M6 (Posterior) superior to M3 | -1 |
| Total ASPECTS Score. | ?/10 |
Assessing
The ASPECTS score has some clinical correlation. A normal brain has a score of 10 and as more areas are affected the score falls. A full MCA territory infarct with CT changes would have a score of 0. A sharp increase independence and death occurs with an ASPECTS of 7 or less. A common misunderstanding of ASPECTS scoring is to assess only two standardised cuts, i.e. one ganglionic cut through the thalamus and one supraganglionic cut above this. Be sure to include the assessment of all axial cuts of the brain NCCT scan. The ASPECT score is not needed prior to thrombolysis but it does give an element of quantitative rigor to assessing the CT analysis and may be mentioned in any discussion with a stroke physician so useful to have heard of it. The aspects does not incorporate ACA and PCA territories but adjacent infarcts may well have clinical implications.
Uses
The ASPECTs scoring system has been utilised in many ways. It has been used to prognosticate for example the score is a strong predictor of functional outcome. It has also been used to direct therapies. The effectiveness of intra-arterial thrombolysis in patients with middle cerebral artery occlusion shows effect modification by the Alberta Stroke Program Early CT Score. Those with a low ASPECTS score suggesting large MCA infarction can be excluded from futile intra-arterial treatments which are unlikely to result in patient functional independence and increases the risk of haemorrhage.
Acute stroke imaging concepts: one suggested system is the 4 P's
- Parenchyma - look for blood and early signs of infarction
- Pipes - look at head and neck vessels if possible and intracerebral vessels for thrombosis or dissection depending on the modality
- Perfusion - depending on modality assess cerebral blood volume and flow and mean transit time
- Penumbra - assess for potentially salvageable tissue
Non contrast CT scan
- Within 24 hours is standard and useful and will reliably exclude primary intracerebral haemorrhage
- An urgent CT is indicated: Anticoagulant treatment, a known bleeding tendency, Depressed level of consciousness
- Unexplained progressive or fluctuating Symptoms
- Papilloedema, Neck stiffness or fever
- Severe headache at onset
- Indications for thrombolysis or early anticoagulation
Changes: Definitive distinctive changes may not occur until 6-8 hrs. In the meantime more subtle signs are seen
- loss of grey-white matter differentiation - seen at the cortical surface due to localised changes such as cytotoxic oedema within the grey matter which has a higher metabolic requirement and so becomes oedematous quicker
- sulcal effacement - suggests some increased oedema
- loss of insular ribbon - similar to loss of grey white differentiation with localised cytotoxic oedema. Vascular supply here is more vulnerable due to poor collateralization and so this may show first
- low density area/hypoattenuation - Hypoattenuation on CT is highly specific for irreversible ischaemic brain damage if it is detected within the first 6 hours
- hyperdense MCA sign or "dot sign" it may be normal is a sign of clot (thrombotic or embolic) (not a contraindication to lysis) but shows the extent of possible infarct which depends also on collateral flow.
- obscuration" of the lentiform nucleus (loss of the normal attenuation difference of the globus pallidus and/or putamen with respect to contiguous white matter structures
- CSF space compression
Changes After 12 hours
- Clearly delineated wedge-shaped hypodense region involving cortex and the adjacent white matter related to the occluded artery anatomy and collaterals. May be some haemorrhagic transformation.
- Estimated HT is up to 40% in the subacute period. Lacunar infarcts were seen deep within white matter and within the basal ganglia
Other findings
- Hypodensity is the main finding and is due to Cytotoxic oedema initially and Vasogenic oedema secondarily and is best seen days 3-10
- Fogging when the density of ischaemic tissue reaches same intensity as normal brain tissue and so evidence of infarction not seen. The late infarcted zone has a density of CSF
Middle cerebral artery
- Hypodense caudate suggests MCA occlusion proximally taking out lenticulostriate arteries
- Depends on leptomeningeal anastomoses of ACA and PCA
- NCCT false negatives: Infarcts when done early or Late haemorrhage after 7-10 days
- NCCT false positives: Lacunar infarcts are common and most often asymptomatic but appear on scans are done for a myriad of reasons so unless there is corresponding new neurology do not diagnose acute stroke but do treat for "stroke disease".
CT angiography
- Allows visualisation of the pipes from the aortic arch to the circle of Willis and so includes head and neck vessels and COW and its branches
- Added value is the identification of vessel occlusion from carotid to COW branches. The extent of collaterals.
- Can help to direct mechanical or systemic or intraarterial thrombolytic therapies
CT Perfusion
- Assess perfusion in a CT slice following an injection of IV contrast an measuring the first pass as the contrast perfuses the brain. Modern scanners can take 10 and more images per second. Multislice scanners allow different slices to be taken simultaneously. A time density curve for each pixel can be generated.
- Can calculate relative cerebral blood flow, relative cerebral blood volume, time to peak and mean transit time which can be displayed in a colour map
- Volume of blood per unit of brain 4-5 ml/100 g
- Flow to grey matter is 50-60 ml/100 g/min
- Transit time is from arterial inflow to venous outflow.
- Time to peak enhancement - beginning of contrast injection to the maximum contrast in the area under study
Magnetic resonance imaging
- Acute ischaemia: T2WI and FLAIR show increased signal which peaks at 7 days and may persist for a month. Diffusion-weighted imaging : This the most sensitive sequence for acute ischaemia as it shows the restriction of diffusion (Brownian motion) of extracellular water due to imbalance caused by cytotoxic oedema within minutes. It can remain bright for up to 3 weeks. Some of the bright area maybe viable. ADC map is initially low signal and then increases in signal later on
- Chronic infarction : DWI shows decreased signal intensity and ADC shows increased ADC values
Magnetic resonance angiography
- Investigation of Haemorrhage e.g. AV Malformations, Aneurysms, AV fistulae, Vasculitis.
- Uses time of flight to image vessels or can use Contrast-enhanced MRA (CEMRA) for improved imaging mainly used for extracranial vessels
Magnetic resonance venography
- Used in the Investigation of CVT
Magnetic resonance perfusion
- Multislice imaging without radiation
- Perfusion weighted T2* images taken following a bolus of Gadolinium every 1-2 seconds for 1-2 minutes
- Calculates time to peak, mean transit time, relative cerebral blood flow, relative cerebral blood volume
CT based studies Penumbra assessment
- Penumbra assumed to have an increased mean transit time with decreased cerebral blood flow (> 60%) and normal or increased cerebral blood volume (80-100%)
- increased mean transit time with a marked reduction in CBF (> 30%) and moderately reduced CBV (> 60%)
- Infarction - severely decreased CBF < 30% and CBV volume < 40% with an increased mean transit time
- CBF = CBV divided by mean transit time
- Penumbra = Map of Cerebral blood volume - Map of Cerebral blood flow
- Measurements are made after the passage of contrast is given through the cerebral circulation
ASPECTS scan
- Assesses MCA infarction at two different axial slices and subtracts -1 from total of 10 for each area affected
- Lentiform nucleus level- M1, M2, M3, Lentiform, Caudate nucleus, Internal capsule, Insular cortex
- Centrum semiovale level - M4, M5, M6
- A score of 0 suggests extensive MCA infarction and correlates inversely with NIHSS
Ultrasound Doppler
- Carotid/Vertebral duplex: Identify stenosis - useful for those with the symptomatic disease for consideration of endarterectomy or stenting. Shows occlusion - due to atheroma/embolism or dissection
- Transcranial: Identifies MCA flow through a temporal bone window. Takes 30-60 minutes. Useful to identify reduced MCA flow with vasospasm post-SAH, Emboli and microemboli seen following agitated saline in those with Right to left shunt. Bilateral TCD can help show emboli origin. Both sides show emboli if cardiac, one side if carotid
CT Interpretation
Definitive distinctive changes may not occur until 6-8 hours. In the meantime, more subtle signs are seen. At about 6 hours and sometimes earlier there may be loss of grey-white matter differentiation - seen at the cortical surface due to localised changes such as cytotoxic oedema within the grey matter which has a higher metabolic requirement and so becomes oedematous quicker. These signs are subtle and can be missed by even the most experienced
| Findings | Explanation |
|---|---|
| Hyperdense Artery or more distal MCA "dot sign" | This may be a sign of large vessel occlusion but does not replace a CTA if needed. The hyperdense vessel sign is most specific but has low sensitivity. Always look at it in context. Some arteries are simply calcified. It may support the diagnosis of large vessel infarct in the clinical context. It is not just seen with the MCA but can also be seen with PCA and basilar arteries. |
| Loss of Grey white differentiation | This is a very important and early sign of ischaemic stroke. The outer cortical surface of the brain has a different appearance to the subcortical grey matter usually. When ischaemic one of the early signs is that this difference begins to be lost. It is often accompanied by oedema |
| Loss of insular ribbon or Obscuration of the Sylvian fissure or Lentiform nucleus | Both signs suggest a sign similar to loss of grey-white differentiation with localised cytotoxic oedema. Vascular supply here is more vulnerable due to poor collateralisation and so this may show first. loss of the normal attenuation difference of the globus pallidus and/or putamen with respect to contiguous white matter structures |
| Hypoattenuation | Hypoattenuation seen on CT is highly specific for irreversible ischaemic brain damage and infarction if it is detected within first 6 hours. It suggests that the patient may not benefit from reperfusion therapies. |
| Wedge shaped infarcts | Clearly delineated wedge shaped hypodense region involving cortex and adjacent white matter related to the occluded artery anatomy and collaterals at 12 hours. Can suggest large artery disease. Often embolic. |
| Lacunes | Small round infacts often in basal ganglia and pons. Usually < 1.5 cm in diameter. Seen with age, diabetes and HTN. |
| Haemorrhagic transformation | Bleeding into brain parenchyma. Many large strokes show some of this in the first fortnight. May be some haemorrhagic transformation. Estimated incidence of haemorrhagic transformation is up to 40% in the subacute period even when not thrombolysed. |
| Watershed infarcts | These occur between vascular territories often bilateral strokes between ACA and MCA territory and MCA and PCA may suggest carotid disease or a systemic drop in BP |
| Fogging | Fogging - density of ischaemic tissue reaches same intensity as normal brain tissue and so evidence of infarction not seen |
| Encephalomalacia | Late changes over weeks and months shows continue as the infarcted zone has density of CSF and there is loss of volume. |


Non contrast CT false negatives (there is a stroke) usually in infarcts when done early or in those who present 7-10 days after stroke and there is a visible hypodensity but no blood and so aetiology of perhaps a small bleed may be missed. In these cases a gradient echo will show haemosiderin deposition around the margins suggesting haemorrhage as he cause.
NCCT false positives are seen particular in older hypertensive patients where Lacunar infarcts are common and most often asymptomatic but appear on scans done for a myriad of reasons so unless there is corresponding new neurology do not diagnose acute stroke but do treat for "stroke disease".
References and reading
- Use of the Alberta Stroke Program Early CT Score (ASPECTS) for Assessing CT Scans in Patients with Acute Stroke
- Barber PA1, Demchuk AM, Zhang J, Buchan AM. Validity and reliability of a quantitative computed tomography score in predicting outcome of hyperacute stroke before thrombolytic therapy. ASPECTS Study Group. Alberta Stroke Programme Early CT Score. Lancet. 2000 May 13;355(9216):1670-4.
- The official ASPECTS score website